Antacids and Antibiotics: How to Time Your Doses to Avoid Dangerous Interactions

When you're on antibiotics and also dealing with heartburn or indigestion, it's easy to grab an antacid without thinking twice. But doing that at the wrong time can make your antibiotic useless. This isn't just a myth - it's a well-documented problem that leads to treatment failures, longer illnesses, and even antibiotic resistance. The truth is, many people don't realize how much timing matters between these two common medications.
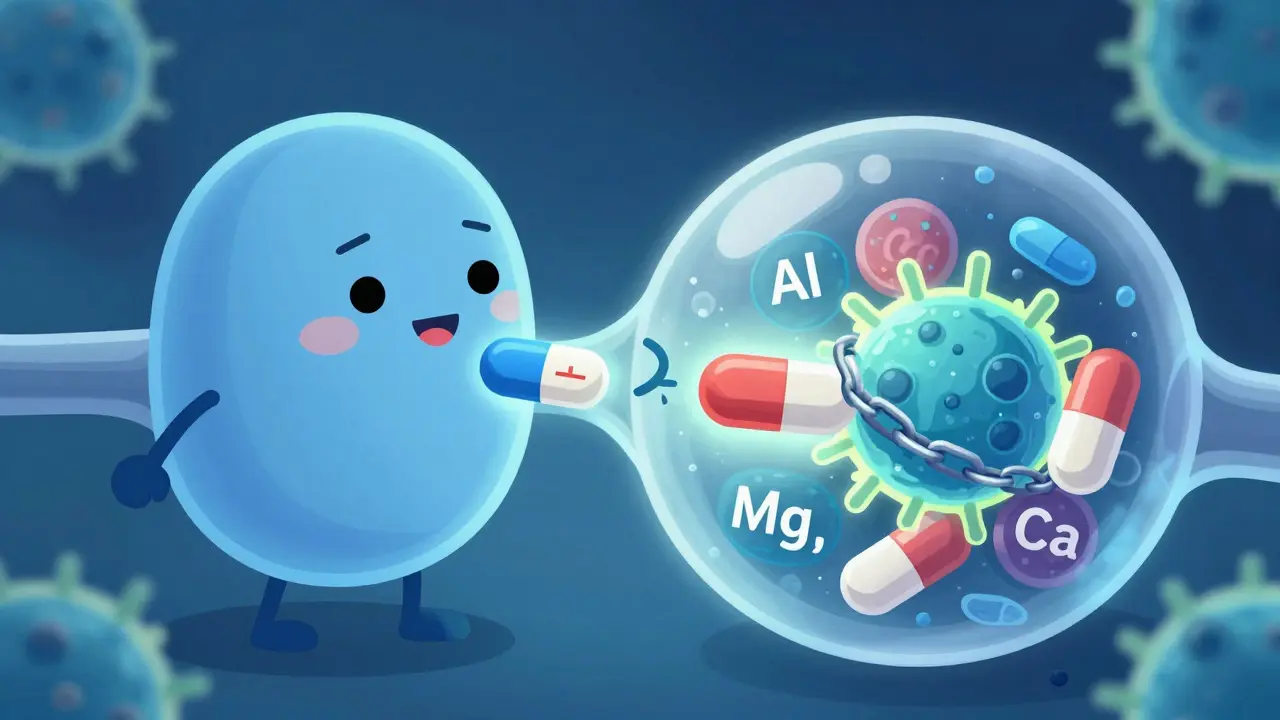
Why Antacids Ruin Antibiotic Effectiveness
Antacids like Tums, Rolaids, Maalox, and Mylanta work by neutralizing stomach acid. That’s great for heartburn, but it’s a disaster for certain antibiotics. The problem isn’t just the change in stomach pH - it’s the minerals inside these antacids. Aluminum, magnesium, and calcium bind directly to antibiotics in your gut, forming a chemical shell that your body can’t absorb.This is called chelation. Think of it like a magnet pulling the antibiotic away from where it needs to go. When you take ciprofloxacin (Cipro) with an antacid containing magnesium, absorption can drop by up to 90%. That means instead of the full dose entering your bloodstream, you’re getting barely enough to do anything. The same thing happens with doxycycline, tetracycline, and other tetracycline-class antibiotics. Even amoxicillin, which is usually considered safe, can lose 15-20% of its effectiveness if taken at the same time.
Studies from the Journal of Antimicrobial Chemotherapy and the NHS confirm this isn’t theoretical. Real patients get sick again because their antibiotics didn’t work - not because the bug was strong, but because the drug never reached the right levels in their blood.
Which Antibiotics Are Most at Risk?
Not all antibiotics react the same way. Some are barely affected. Others are extremely vulnerable. Here’s what you need to know:- Fluoroquinolones (ciprofloxacin, levofloxacin, moxifloxacin): These are the most sensitive. Taking them with antacids can slash absorption by 75-90%. The NHS recommends waiting 4 hours after taking an antacid before taking these antibiotics - or taking the antibiotic 2 hours before the antacid.
- Tetracyclines (doxycycline, tetracycline): These are also heavily affected. Studies show up to 70% less absorption when taken together. You need at least a 2-3 hour gap.
- Macrolides (azithromycin, clarithromycin): Minimal interaction, but still best to separate by 2 hours as a safety buffer.
- Beta-lactams (amoxicillin, cephalexin): Only a small drop in absorption (15-25%). A 1-2 hour gap is usually enough.
- Metronidazole: No significant interaction. You can take this with antacids without timing issues.
Here’s a quick reference for timing:
| Antibiotic Class | Examples | Interaction Severity | Recommended Separation Time |
|---|---|---|---|
| Fluoroquinolones | Ciprofloxacin, Levofloxacin | Severe (75-90% reduction) | 4 hours after antacid, or 2 hours before |
| Tetracyclines | Doxycycline, Tetracycline | High (50-70% reduction) | 2-3 hours before or after |
| Beta-lactams | Amoxicillin, Cephalexin | Mild (15-25% reduction) | 1-2 hours before or after |
| Macrolides | Azithromycin, Clarithromycin | Low | 2 hours before or after |
| Metronidazole | Metronidazole | None | No separation needed |
What Happens When You Ignore the Timing?
Ignoring the separation window doesn’t just mean your infection might not clear up. It can make things worse.A 2021 FDA analysis of 15,000 patients found that those who took ciprofloxacin with antacids had a 22% higher chance of treatment failure for urinary tract infections. That’s not a small number. It means over one in five people got sick again - not because they were resistant, but because they took their pill the wrong way.
On Reddit, a doctor shared that five patients in one year had recurring UTIs - all because they took Cipro with Tums. Once they spaced the doses, the infections cleared. A similar story appears in 68% of patient reviews on Drugs.com where people reported initial treatment failure that resolved only after adjusting timing.
And it’s not just about one infection. When antibiotics don’t work properly, bacteria survive and adapt. The CDC estimates that 15% of emerging fluoroquinolone resistance is linked to subtherapeutic drug levels caused by these interactions. That’s not just bad for you - it’s bad for everyone.
How to Actually Get the Timing Right
Knowing the rules is one thing. Following them when you’re juggling pills, meals, and daily life is another.Here’s how to make it work:
- Write it down. If you take antibiotics twice a day and antacids after meals, sketch out a simple chart: "Take doxycycline at 8 AM, breakfast at 8:30 AM, antacid at 10 AM - wait until 12 PM for next antibiotic dose."
- Use your phone. Apps like MyMedSchedule have built-in alerts for antacid-antibiotic interactions. They’ll remind you when it’s safe to take each pill. Over 1.2 million people use this app.
- Ask your pharmacist. Pharmacists are trained to catch these mistakes. One patient on Amazon Pharmacy said their pharmacist spotted their timing error - and their acne cleared up completely after fixing it.
- Plan around meals. Most antibiotics are best taken on an empty stomach. So take your antibiotic at least 1 hour before eating, then wait 2-4 hours before taking an antacid. That naturally builds in separation.
- Use visual aids. Mayo Clinic found that patients given a simple printed timeline showing "safe windows" made 37% fewer timing errors.
If you’re on antacids multiple times a day, talk to your doctor about switching to H2 blockers (like famotidine) or proton pump inhibitors (like omeprazole). These drugs don’t contain aluminum or magnesium, so they’re much safer with antibiotics. A 2023 study showed switching cut treatment failure rates from 27% to just 9%.
What About Other Medications?
Antacids don’t just interfere with antibiotics. They also reduce absorption of thyroid meds, iron supplements, bisphosphonates (for osteoporosis), and some antifungals. If you’re on any of these, check with your doctor or pharmacist before combining them with antacids.And don’t assume "natural" antacids are safer. Calcium carbonate (found in Tums) is just as problematic as aluminum or magnesium. Even calcium-based antacids need a 4-hour gap with fluoroquinolones.
What’s Changing in 2025?
The good news? Things are getting better. In 2023, the FDA approved a new extended-release form of ciprofloxacin called Cipro XR-24. In trials, it showed only 8% reduction in absorption when taken with antacids - compared to 90% for the old version. That’s a game-changer.Electronic health records now automatically flag these interactions. Epic Systems rolled out a new module in March 2023 that doesn’t just say "interaction possible" - it tells you exactly how long to wait. Hospitals using it saw a 41% drop in timing errors.
And research is moving toward personalized timing. A 2023 study at the University of Pittsburgh found that people with certain genetic variants empty their stomachs faster or slower. In the future, your antibiotic timing might be tailored to your biology - not just a one-size-fits-all rule.
Bottom Line: Don’t Guess. Time It Right.
You’re taking antibiotics to get better. You’re taking antacids to feel better. But if you take them at the same time, you’re doing both a disservice. The fix isn’t complicated: space them out.For fluoroquinolones: wait 4 hours after an antacid, or take the antibiotic 2 hours before.
For doxycycline: wait 2-3 hours.
For amoxicillin: 1-2 hours is fine.
And if you’re ever unsure - ask your pharmacist. It takes 30 seconds. It could save you a week of feeling sick.
Can I take antacids and antibiotics at the same time if I really need to?
No - not if you want your antibiotic to work. Taking them together can cut absorption by up to 90% for drugs like ciprofloxacin and doxycycline. Even if you feel fine, the drug isn’t reaching the levels needed to kill the infection. This can lead to treatment failure and contribute to antibiotic resistance.
What if I forget and take them together by accident?
If you realize right away (within 30 minutes), you can wait 2-4 hours and take another dose of your antibiotic - but only if your doctor or pharmacist says it’s safe. Don’t double up without advice. If it’s been longer than an hour, skip the extra dose and just get back on schedule. One mistake won’t ruin everything, but repeated mistakes will.
Do all antacids cause the same problem?
No. Antacids with aluminum, magnesium, or calcium are the main culprits. Calcium carbonate (like in Tums) is just as bad as magnesium hydroxide. But antacids that don’t contain these minerals - like sodium bicarbonate - have less impact. Still, it’s safest to assume all antacids interfere unless proven otherwise. Switching to famotidine or omeprazole is a better long-term solution.
Is it safe to take antacids after finishing my antibiotic course?
Yes. Once you’ve finished your full course of antibiotics, there’s no interaction risk. Antacids won’t affect the drug once it’s already been absorbed and done its job. You can resume regular use after your last antibiotic dose.
What should I do if I’m on multiple medications?
Keep a list of everything you take - including over-the-counter meds, vitamins, and supplements - and bring it to your pharmacist. Many drugs interact with antacids, not just antibiotics. Iron, thyroid meds, and bone drugs like alendronate are also affected. A pharmacist can help you build a safe daily schedule that avoids all interactions.

11 Comments
Wow, this is one of those posts that makes you realize how much we just blindly trust pills without knowing what they’re actually doing inside us. I used to take Tums with my doxycycline like it was cereal and milk-now I feel like a dumbass. Thanks for laying it out so clearly. 🙏
I had no idea antacids could mess with antibiotics like that. My grandma takes Tums after every meal and was on cipro last year for a UTI. She got sick again a week later. Now I’m gonna print this out and tape it to her medicine cabinet.
People who just pop antacids like candy are basically feeding antibiotic resistance. It’s not just ‘oops I forgot’-it’s a public health crime. If you can’t follow a 2-hour window, maybe you shouldn’t be self-medicating with calcium carbonate like it’s candy. #StopBeingLazy
This is such a helpful breakdown-I’m so glad you included the specific timing windows and alternatives like famotidine. I’ve been recommending this to my patients for years, but most don’t remember it. Printing the table and keeping it by their meds? Genius. You’ve made a real difference here.
USA has the best doctors, the best pharma, the best science-and yet, people still take Tums with Cipro like it’s nothing?? This is why we’re falling behind. I’ve seen this in my own family. It’s not ignorance-it’s laziness. And it’s killing us. 🇺🇸
bro i live in india and we just swallow whatever pill we have. my cousin took cipro with digel and got worse. then he went to a local clinic and they said 'maybe your body is weak' lol. this post is a godsend. saved my ass.
Wait so if I take omeprazole instead of Tums, I’m good? I’ve been on acid reflux meds for 3 years and just started doxycycline last week… should I panic? 😅
Thank you for this!! I just had a UTI and was on cipro-I took Tums because I was nauseous. Now I’m terrified I ruined everything… but I didn’t know any better! I’ll switch to omeprazole now. Also, the part about genetic differences in stomach emptying? Mind blown. 🤯❤️
While the pharmacokinetic data presented here is statistically robust and clinically validated, one must consider the broader epistemological framework of pharmaceutical compliance in post-industrial societies. The phenomenon of self-medication with antacids reflects a systemic erosion of medical literacy, exacerbated by algorithmic misinformation and the commodification of health. One might even posit that the ubiquity of calcium carbonate products in convenience stores represents a neoliberal pathology-where symptom suppression is prioritized over root-cause resolution. The FDA’s 2023 EHR integration, while commendable, remains a Band-Aid on a hemorrhage. We must re-educate the public not merely on timing, but on the ontological nature of pharmacological intervention.
So you’re telling me I’ve been sabotaging my own treatment for years? I took cipro with Rolaids like a champ for three weeks. No wonder my UTI came back worse. I’m not even mad-I’m just impressed by how dumb I was. Thanks for the wake-up call. I’m switching to omeprazole today.
So… can I take antacids after my last antibiotic dose? 😊