Anticholinergics and Urinary Retention: How Prostate Problems Make This Medication Risky

Urinary Retention Risk Calculator
This tool helps you assess your risk of urinary retention when taking anticholinergic medications based on prostate health and medical history. For best results, consult with your doctor before making any medication changes.
Why Anticholinergics Can Be Dangerous for Men with Prostate Problems
If you’re a man over 60 and your doctor prescribed an anticholinergic for an overactive bladder, you might not realize you’re putting yourself at serious risk. These drugs - like oxybutynin, tolterodine, and solifenacin - are meant to stop sudden bladder spasms. But for men with an enlarged prostate, they can turn a manageable condition into a medical emergency.
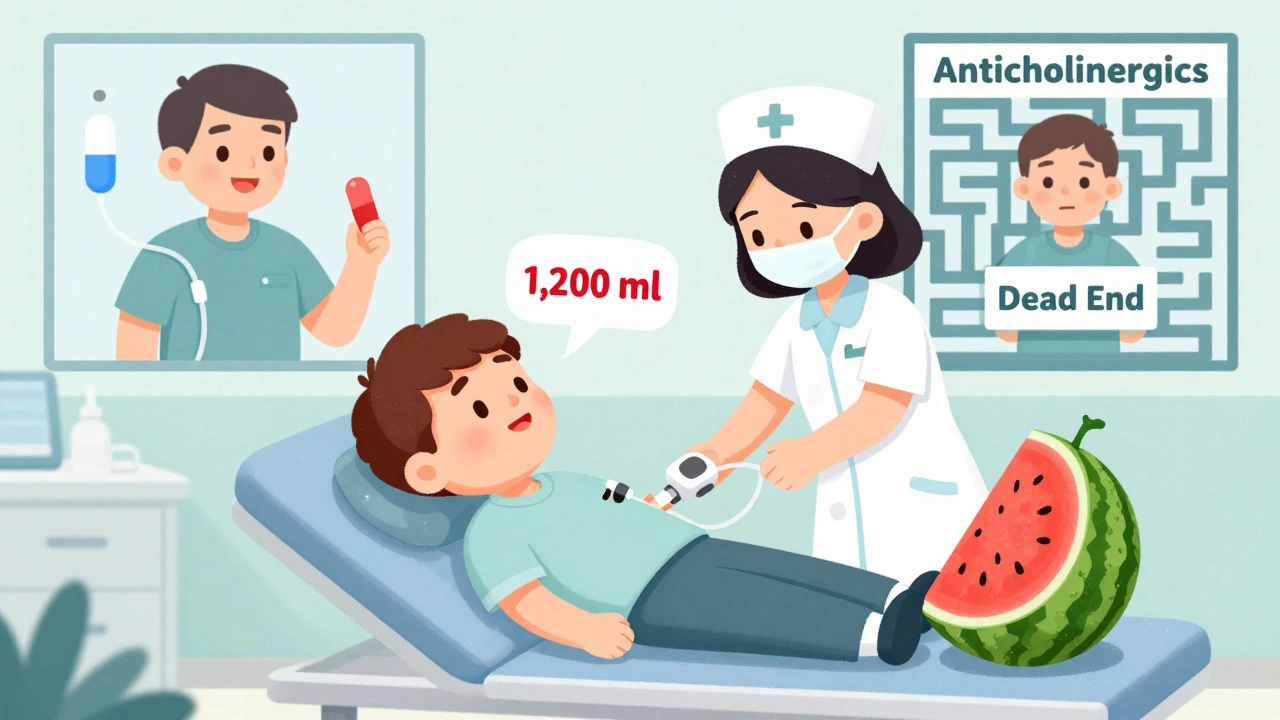
Anticholinergics work by blocking a chemical in your body called acetylcholine. That chemical tells your bladder to squeeze and empty. When it’s blocked, the bladder doesn’t contract as strongly. That sounds good if you’re leaking urine, but if your prostate is already squeezing your urethra shut, this is like turning down the engine on a car stuck in mud. The result? You can’t pee at all.
What Happens When Your Bladder Can’t Empty
Urinary retention isn’t just inconvenience. It’s when your bladder fills up but can’t drain. Acute retention means you suddenly can’t pee at all - even with a full bladder. Chronic retention means you’re always leaving behind urine, which can lead to infections, kidney damage, or even bladder rupture.
Studies show that up to 10% of all urinary retention cases are caused by medications - and anticholinergics are the top offenders. In men with benign prostatic hyperplasia (BPH), the risk jumps to 2.3 times higher than in men not taking these drugs. The American Urological Association says this isn’t just a theory - it’s a proven danger.
One patient on a prostate forum described it this way: "I took Detrol for urgency. Three days later, I was in the ER with a bladder full of 1,200 ml of urine - the size of a small watermelon. They had to stick a catheter in me. I’ve been on one ever since."
Who’s Most at Risk?
You don’t have to be old to be at risk, but age makes it worse. Men over 65 with an enlarged prostate are the most vulnerable. So are men who take multiple medications - especially those for depression, allergies, or Parkinson’s - because many of those also have anticholinergic effects.
Doctors can spot high-risk patients before prescribing. A digital rectal exam shows if the prostate is enlarged. A uroflow test measures how fast urine comes out - if your peak flow is below 10 mL per second, you’re in the danger zone. A post-void residual test checks how much urine is left after you go. If it’s over 150 mL, anticholinergics are a bad idea.
The American Geriatrics Society’s Beers Criteria lists anticholinergics as "potentially inappropriate" for older adults with BPH or urinary retention. Yet, a 2021 study found that 40% of nursing home residents with these conditions are still getting these drugs. That’s not oversight - it’s a systemic blind spot.
Why the Benefits Don’t Outweigh the Risks
Let’s be clear: anticholinergics do work - for some people. The Cochrane Review analyzed 51 studies with over 6,700 patients. They found these drugs reduce incontinence episodes by about one per 48 hours compared to placebo. That’s a 15% improvement. Sounds good? Maybe - until you realize that for every seven men treated, only one gets meaningful relief.
And the side effects? Dry mouth? Common. Constipation? Frequent. Blurred vision? Happens. But the real danger is urinary retention - reported in 8 to 15% of users. That’s one in every eight to twelve men. For someone with BPH, that risk isn’t just possible - it’s likely.
And it’s not just the bladder. The FDA has warned since 2012 that anticholinergics can cause memory loss, confusion, and even increase dementia risk in older adults. So you’re trading a bladder problem for a brain problem. That’s not a fair trade.
What to Use Instead
There are better, safer options - especially for men with BPH.
- Alpha-blockers like tamsulosin (Flomax) or alfuzosin (Uroxatral) relax the muscles around the prostate and bladder neck. They help urine flow without weakening the bladder. Studies show men on alpha-blockers after catheterization are 30-50% more likely to pee on their own within a few days.
- 5-alpha reductase inhibitors like finasteride (Proscar) and dutasteride (Avodart) shrink the prostate over time. After four to six years, they cut the risk of acute retention by half.
- Beta-3 agonists like mirabegron (Myrbetriq) and vibegron (Gemtesa) work differently. Instead of blocking signals, they stimulate a different receptor that helps the bladder relax and store more urine. Clinical trials show they reduce urgency just as well as anticholinergics - but with only a 4% retention rate in men with BPH, compared to 18% with anticholinergics.
The FDA approved vibegron in 2020 specifically for patients with BPH who can’t take anticholinergics. That’s not an accident. It’s a signal - the medical community is moving away from these risky drugs.
What If You’re Already Taking One?
If you’re on an anticholinergic and have BPH, don’t stop cold turkey. Talk to your doctor. Ask for a uroflow test and a post-void residual check. If your flow is slow or you’re leaving behind a lot of urine, you’re in danger.
Some doctors will try to keep you on a low dose if your symptoms are mild and you’re monitored closely. But even then, you need monthly checkups. One Reddit user wrote: "My urologist put me on low-dose Vesicare and checked my flow every month. It worked - no retention. But I’m the exception, not the rule."
Most men aren’t so lucky. The data shows that 70% of men who get catheterized for retention will have it happen again within a week - unless they start an alpha-blocker right away. That’s why guidelines now say: catheterize, then start tamsulosin. Don’t just drain the bladder - fix the root problem.
The Bottom Line: It’s Not Worth the Risk
Anticholinergics were once seen as a simple fix for overactive bladder. But for men with prostate issues, they’re a trap. The benefits are small. The risks are huge. And the alternatives are safer, more effective, and designed specifically for your condition.
If you’re a man with BPH and your doctor suggests an anticholinergic, ask: "Is there a better option?" Push for a uroflow test. Ask about vibegron or tamsulosin. If they say, "It’s the only thing that works," they’re not up to date.
Medicine has moved on. You should too. Your bladder - and your kidneys - will thank you.
Frequently Asked Questions
Can anticholinergics cause permanent bladder damage?
Yes, if urinary retention is left untreated for too long. When the bladder is stretched beyond its limit for days or weeks, the muscle can become permanently weak. This is called detrusor underactivity. Once that happens, you may need lifelong catheterization or surgery to manage urine flow. Early intervention with catheterization and alpha-blockers can prevent this.
Are all anticholinergics equally risky?
No, but none are safe for men with BPH. Drugs like solifenacin and darifenacin are marketed as "more selective," meaning they target the bladder more than the brain. But even these still block bladder contractions. A 2017 study found that even in carefully selected men with mild BPH, 12% still had retention on solifenacin. That’s not low risk - it’s still dangerous.
What should I do if I suddenly can’t urinate?
Go to the ER immediately. Acute urinary retention is a medical emergency. Do not wait. Do not try to force it. Emergency catheterization is the only safe solution. Once your bladder is drained, ask for a urology consult and request an alpha-blocker like tamsulosin to help you void again.
Can women with BPH take anticholinergics?
Women don’t have BPH - that’s a male-specific condition. But women can have urinary retention from other causes, like pelvic organ prolapse or nerve damage. Anticholinergics can still cause retention in women, especially older ones. The same caution applies: test bladder function before prescribing, and avoid these drugs if retention is already a problem.
Are there natural alternatives to anticholinergics?
There’s no natural remedy proven to replace anticholinergics for overactive bladder. Saw palmetto helps with BPH symptoms like frequency, but it doesn’t stop bladder spasms. Pelvic floor physical therapy, timed voiding, and bladder training are non-drug options that work well for many men. They’re safe, free, and don’t carry the risk of retention.
How do I know if my prostate is enlarged?
Your doctor can check with a digital rectal exam - it’s quick and uncomfortable, but necessary. An ultrasound can measure prostate size - anything over 30 grams is considered enlarged. You might also have symptoms like weak stream, straining to pee, or feeling like you haven’t fully emptied. If you’re over 50 and have these, get checked.
What to Do Next
If you’re taking an anticholinergic and have prostate symptoms, schedule a urology appointment. Bring your medication list. Ask for a uroflow test and post-void residual measurement. If you’re over 65, ask if your meds are on the Beers Criteria list.
Don’t wait for an emergency. If you’ve had even one episode of trouble peeing after starting one of these drugs, you’re already at risk. Talk to your doctor about switching to vibegron, tamsulosin, or behavioral therapy. Your bladder doesn’t need another drug - it needs a smarter plan.

16 Comments
I had no idea this was such a hidden danger. My dad was on oxybutynin for years and never told us he was struggling to pee until he ended up in the ER. I wish doctors would screen for BPH before prescribing these. So many lives could be saved with just a simple question.
This is why America’s healthcare system is broken-doctors are incentivized to prescribe pills, not to think! We’ve outsourced common sense to Big Pharma, and now grandpa’s bladder is a liability instead of a biological marvel. The FDA? A corporate puppet. The Beers Criteria? A whisper in a hurricane. Alpha-blockers? Sure, but why not just drink less coffee and squat? We’ve forgotten how to listen to our bodies-because convenience is king, and truth is a liability.
The pharmacological paradigm shift here is fascinating-moving from suppression to facilitation. Anticholinergics inhibit parasympathetic signaling, which, while effective for detrusor overactivity, ignores the biomechanical obstruction inherent in BPH. Beta-3 agonists, by contrast, engage the sympathetic-mediated relaxation pathway via the bladder’s detrusor smooth muscle. This isn’t just a drug swap-it’s a neurophysiological reorientation. We’re moving from antagonism to modulation. And yet, the clinical inertia persists, largely due to inertia in medical education and formulary constraints.
Oh please. You think vibegron is some miracle drug? It’s just a rebranded version of the same old nonsense. My cousin took it for six months and still had to catheterize himself twice. And let’s not pretend tamsulosin doesn’t give you dizzy spells and retrograde ejaculation. The real problem? Doctors don’t listen. They read the bullet points and click ‘prescribe.’ You want a real solution? Cut out the caffeine, do Kegels, and stop being a lazy sack of urine.
In India, we do not rely on pills to fix what our ancestors solved with discipline. We drink warm water, avoid cold drinks after meals, and practice yoga poses like Vajrasana. This Western obsession with pharmaceutical quick fixes is a sign of cultural decay. Why not teach men to control their bladder through mindfulness? Instead, we pump them full of chemicals and call it progress. This is not medicine-it is surrender.
I swear to god I saw a post on TikTok about this and everyone was like ‘OMG THIS IS A TRAP’ and then the comments were full of people saying ‘I got cathed and now I’m a walking catheter’ 😭😭😭
I’m a nurse in geriatrics. I’ve seen this play out too many times. A man comes in with ‘bladder issues,’ gets anticholinergics, then shows up two weeks later in full retention. We catheterize him, and then-here’s the kicker-he’s never asked if he has BPH. Never. It’s like we’re playing medical whack-a-mole. But when we switch them to tamsulosin? They walk out smiling. Simple. Effective. Human.
They’re hiding this from us. I’m telling you-Big Pharma is funding studies that say ‘it’s fine’ and silencing the ones that don’t. You think your doctor really cares? They get kickbacks. You think the FDA is independent? Ha. Wake up. This is how they control the elderly. Slowly. Quietly. One catheter at a time.
You’re not alone. I was so scared after my husband’s catheter incident. But we found a urologist who actually listened. We started pelvic floor PT and switched to mirabegron. He’s been dry for 11 months now. It’s not magic, but it’s hope. And hope is the best medicine.
In my culture, elders are treated with reverence-and their bodies are respected. We don’t just throw pills at problems. We sit with them. We ask: ‘What are you eating? Are you sleeping? Do you feel safe?’ This article reminds me that medicine must include dignity. Not just dosage.
It is imperative to underscore the necessity of rigorous clinical evaluation prior to the administration of any anticholinergic agent in geriatric male populations. The confluence of pharmacokinetic alterations, age-related detrusor dysfunction, and comorbid polypharmacy renders this population uniquely susceptible to iatrogenic urinary retention. The failure to conduct post-void residual assessments constitutes a deviation from the standard of care.
I’ve seen this in my practice as a physiotherapist. Men are so reluctant to talk about bladder issues. They’ll suffer for months because they’re embarrassed. But once they’re educated, they’re empowered. This isn’t just about drugs-it’s about breaking the silence. Thank you for writing this. It’s a lifeline.
It’s interesting how we treat bladder function like it’s separate from the rest of the body. But it’s not. It’s connected to nerves, hormones, stress, even gut health. Maybe we’re over-medicalizing a natural part of aging. What if we focused more on hydration timing, diet, and pelvic strength instead of blocking signals? Not to say drugs have no place-but maybe they’re not the first answer.
The scientific literature is unequivocal. Anticholinergics significantly elevate the risk of acute urinary retention in men with benign prostatic hyperplasia, as demonstrated by multiple randomized controlled trials and meta-analyses. The American Urological Association guidelines are clear: avoidance is recommended. The continued prescription of these agents constitutes a preventable iatrogenic hazard.
You think this is bad? Wait till you find out what they’re doing to women with pelvic floor disorders. They’re pushing Botox injections into the bladder now. It’s all about profit. They don’t care if you’re leaking, blocked, or catheterized-just as long as you keep buying. Wake up. This isn’t healthcare. It’s a casino.
I just talked to my dad’s urologist after reading this. He’s switching him to vibegron next week. I cried. Not because it’s a miracle-but because it took 4 years and one ER trip for someone to finally listen. Thank you for making this visible.