Barcode Scanning in Pharmacies: How It Stops Wrong Medications from Reaching Patients

Every year, over 1.3 million medication errors happen in U.S. hospitals - and most of them are preventable.
Imagine this: a patient gets a prescription for levothyroxine, a thyroid hormone. But instead of the 25 mcg dose they need, they’re handed a 100 mcg pill. That’s four times the right amount. One wrong dose. One missed scan. One life changed - or lost. This isn’t hypothetical. It’s happened. And it’s why barcode scanning in pharmacies isn’t just a tech upgrade - it’s a safety lifeline.
Barcodes on medicine bottles and patient wristbands don’t just make inventory easier. They stop errors before they happen. When a pharmacist scans a pill bottle and a patient’s wristband at the same time, the system checks: Is this the right drug? The right dose? The right patient? The right time? If anything’s off, it screams. No guesswork. No memory lapses. No rushing through a busy shift.
How barcode scanning actually works in a pharmacy
It’s simple, but powerful. Every prescription medication sold in the U.S. has a National Drug Code (NDC) barcode printed on its packaging. This isn’t just a random string of lines - it’s a digital ID that tells the system exactly what’s inside: the drug name, strength, manufacturer, and lot number.
When a pharmacist pulls a medication to fill a prescription, they scan the barcode on the bottle. At the same time, they scan the patient’s wristband - which has the patient’s name, medical record number, and allergies. The pharmacy software compares both scans against the electronic prescription in the system. If everything matches, the screen turns green and says, “Approved.” If it doesn’t - say, the patient’s order was for insulin glargine but the bottle scanned is insulin lispro - the system stops everything. It flashes red. It sounds an alarm. It won’t let the pharmacist proceed until the issue is cleared.
This is called Barcode Medication Administration (BCMA). It’s not magic. It’s math. And it works. A 2021 study in BMJ Quality & Safety found that when used correctly, BCMA prevents 93.4% of potential dispensing errors. That’s not a guess. That’s data from real hospitals.
What errors does it actually stop?
Not all mistakes are the same. Some are obvious. Some are sneaky. Here’s what barcode scanning catches most often:
- Wrong patient - 92% of these errors are blocked. A patient named Linda gets John’s blood thinner. The system catches it because the wristband doesn’t match the prescription.
- Wrong drug - 89% prevented. A nurse reaches for metoprolol but grabs metformin. The barcode says “no.”
- Wrong dose - 86% stopped. Someone orders 5 mg of warfarin. The bottle says 10 mg. The system flags it.
- Wrong route - Say a pill is meant to be swallowed but someone tries to inject it. The system knows. It’s programmed to match the route on the prescription.
- Wrong time - Medications scheduled for 8 a.m. can’t be scanned and given at 5 p.m. unless the system allows it.
These aren’t rare. A Pennsylvania hospital tracked this: before barcode scanning, 13.5% of doses were given incorrectly. After? Down to 3%. That’s a 75% drop in errors - all because a machine checked two barcodes.
Why manual checks aren’t enough
Many pharmacies still rely on the “double-check” system - two people look at the same bottle and say, “Looks right.” Sounds safe, right? It’s not.
Studies show human double-checks catch only about 36% of errors. Why? Fatigue. Distractions. Assumptions. If you’ve seen the same bottle a hundred times, your brain stops paying attention. You see “metoprolol” and assume it’s 25 mg - even if it’s 50 mg. The barcode doesn’t assume. It reads.
And here’s the kicker: when pharmacists do double-checks, they often skip scanning the patient’s wristband. They assume the patient is who they say they are. That’s how wrong-patient errors slip through. Barcodes don’t make assumptions. They verify.
The hidden flaws - and how to fix them
Barcode scanning isn’t perfect. And pretending it is leads to dangerous habits.
First, barcodes can be damaged. Insulin pens, ampules, and small vials often have tiny, smudged, or peeling labels. When a barcode won’t scan, some pharmacists just type in the NDC manually - skipping the safety check. That’s called a “workaround.” And it’s a major problem. According to the ECRI Institute, 15% of scanning failures happen because the barcode is unreadable. But 68% of hospitals still allow staff to bypass the system without proper verification.
Here’s what works: when a barcode won’t scan, stop. Don’t type. Don’t guess. Look at the bottle. Compare the printed name and strength to the prescription. If it matches, document why you skipped the scan. If it doesn’t, don’t dispense. This is the rule the Pennsylvania Patient Safety Authority and ISMP both insist on.
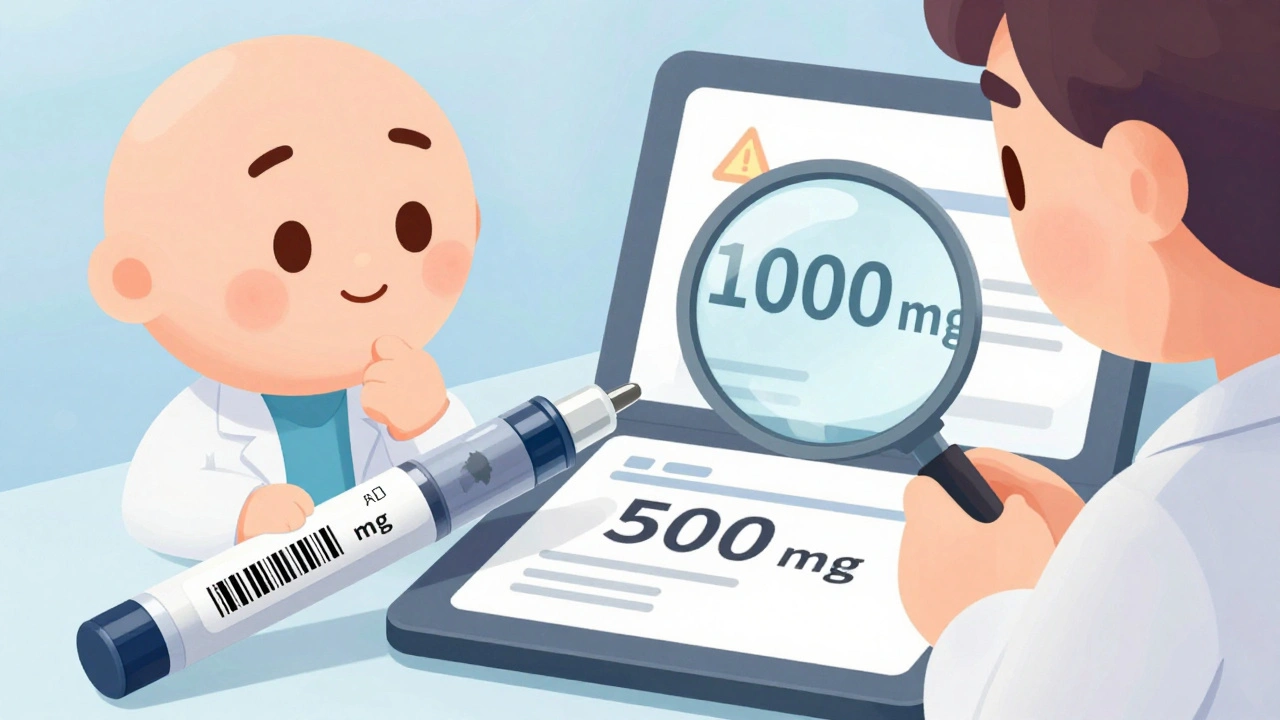
Another issue: labels applied by the pharmacy can be wrong. A pharmacy tech mislabels a vial of vancomycin as 500 mg when it’s actually 1 gram. The barcode on that label is correct - because it matches the label. But the drug inside is wrong. The system scans it, says “approved,” and the error goes unnoticed. That’s why experts say: always scan the manufacturer’s barcode, not the pharmacy’s label. The original packaging is the source of truth.
What about community pharmacies?
Most of the data on barcode scanning comes from hospitals. But what about your local pharmacy?
Only about 35% of community pharmacies use BCMA. Why? Cost. The hardware - scanners, mobile devices, software licenses - can run $15,000 to $50,000. For a small pharmacy, that’s a big investment. And the FDA’s barcode rule only applies to hospital and institutional drug packaging, not retail bottles.
But here’s the thing: dispensing errors happen in community pharmacies too. A 2023 survey of 1,247 pharmacists found that 78% saw fewer errors after scanning - even in retail settings. And the cost of one error? A lawsuit, a lost license, or worse. Many independent pharmacies are starting to adopt it, especially as vendors offer cloud-based, subscription models instead of big upfront payments.

What’s next? 2D barcodes and AI
The future of barcode scanning isn’t just more lines. It’s more data.
Right now, most barcodes are 1D - the thin lines you’ve seen for decades. But 2D matrix codes (like QR codes) can hold way more info: expiration date, lot number, even temperature history. The FDA is already testing 2D barcodes on new medications. By 2026, the American Society of Health-System Pharmacists predicts 65% of drugs will use them - up from just 22% in 2023.
And AI is coming. Cerner’s 2025 update will use machine learning to predict which barcodes are likely to fail - and suggest better scanning angles before the pharmacist even tries. Epic Systems’ new mobile app lets pharmacists scan from their phones, cutting scan time by 22%.
These aren’t sci-fi ideas. They’re happening now. And they’re making the system even tighter.
Real stories - what patients and pharmacists say
A pharmacist in Austin told me last month: “We had a patient come in for a refill of levothyroxine. The system flagged it - the dose had been changed from 50 mcg to 75 mcg. The doctor had updated it, but the old label was still on the bottle. We caught it before the patient left. That’s what this system does.”
On Reddit, a pharmacy tech wrote: “We lose 20 minutes a shift because insulin pens won’t scan. But I’d rather wait than give someone the wrong dose.”
Another said: “BCMA saved me from myself. I was tired. I almost gave a patient the wrong antibiotic. The system stopped me. I didn’t even realize I’d made the mistake.”
These aren’t outliers. They’re the norm in places that use the tech right.
Bottom line: It’s not about tech - it’s about trust
Barcode scanning doesn’t make pharmacists obsolete. It makes them safer. It doesn’t replace judgment - it supports it. It doesn’t eliminate human error - it catches it before it hurts someone.
Technology alone won’t fix safety. But when you combine a reliable barcode system with trained staff, clear protocols for failed scans, and a culture that never lets workarounds slide - that’s when errors drop. That’s when lives are saved.
Every time a barcode scans correctly, a patient gets the right medicine. Every time it stops a mistake, someone goes home healthy. That’s the real value - not in the scanner, but in the silence after the alarm doesn’t sound.
Do all pharmacies use barcode scanning?
Most U.S. hospitals (78%) use barcode scanning, but only about 35% of community pharmacies do. Hospitals are required to follow strict safety standards, while smaller pharmacies often skip it due to cost. However, adoption is growing as cloud-based systems become more affordable.
Can barcode scanning prevent every medication error?
No. It prevents 93% of errors tied to wrong drug, dose, patient, or time - but not all. It can’t detect if a pill is crushed, if a liquid is contaminated, or if a label was incorrectly printed by the pharmacy. Visual verification is still required when barcodes fail or when medications don’t have standard packaging.
What happens if a barcode won’t scan?
Never type the NDC manually to bypass the system. Stop. Look at the actual medication. Compare the printed name and strength to the prescription. If they match, document why you skipped the scan and proceed. If they don’t, don’t dispense. The ECRI Institute and ISMP both say visual verification is mandatory when scanning fails.
Are 2D barcodes better than traditional ones?
Yes. 2D barcodes (like QR codes) hold more data - expiration dates, lot numbers, even storage conditions. They’re harder to damage and can be scanned from any angle. By 2026, over 65% of medications are expected to use them, replacing older 1D barcodes.
Is barcode scanning worth the cost for small pharmacies?
Yes, if you want to reduce liability and improve safety. One error can cost more than the system. Many vendors now offer subscription-based models with no upfront hardware costs. The American Society of Health-System Pharmacists recommends scanning even in retail settings - especially for high-risk drugs like insulin, anticoagulants, and opioids.

15 Comments
I've seen this in action at my mom's hospital. She was on blood thinners and the system flagged a dose mismatch even though the nurse swore it was right. That beep saved her life. No hype, just facts. This tech is quiet hero work.
And yeah, the insulin pens? Annoying as hell when they don't scan. But I'd rather wait 30 seconds than kill someone.
Barcodes? Please. My cousin works at a pharmacy and says half the time the scanners are broken and they just type it in. This whole thing is a scam to sell more hardware.
Correction: the BMJ study found 93.4% reduction in *potential* dispensing errors - meaning errors that were caught before reaching the patient. That’s critical context. Also, 2D barcodes are already live on insulin vials from Eli Lilly and Novo Nordisk. The FDA’s push is real, not theoretical.
So now we’re trusting machines over trained professionals? Next they’ll scan our coffee orders to make sure we don’t drink too much caffeine. This is American healthcare turning into a dystopian checklist.
It’s funny how we’re scared of machines making mistakes but okay with humans zoning out after 12 hours of filling prescriptions. The barcode doesn’t get tired. It doesn’t assume. It doesn’t think, 'Oh, that’s metoprolol, it’s probably 25mg.' It just reads. Maybe the problem isn’t the tech - it’s our pride.
I just scanned my OTC ibuprofen at CVS and it beeped. I thought it was gonna call the cops 😅
barcodes r great until u realize half the labels r printed wrong by the pharmacy themselves. then u got a system that just confirms a lie. lol
In India, we don’t have this tech in most pharmacies. But we do have pharmacists who remember every patient’s meds, allergies, even their kids’ names. Maybe we need less tech and more human connection? Not saying barcodes are bad - but maybe we’re over-indexing on them because we’ve lost trust in each other.
The biggest flaw isn’t the barcode - it’s the workaround culture. When staff bypass the system because 'it’s too slow' or 'the label is smudged,' they’re not being efficient. They’re gambling with lives. And hospitals that allow it are complicit. This isn’t about cost. It’s about values.
Ugh. Another tech bro piece pretending scanners are the savior. Meanwhile, nurses are still getting yelled at for taking 30 extra seconds to verify meds. The real problem? Understaffing. Not barcodes. Fix the staff-to-patient ratio first. Then maybe the scanners won’t be a band-aid on a hemorrhage.
I’m a pharmacy tech in rural Ohio. We got our scanner 3 years ago. Cost us $18k. We’ve prevented 11 wrong-dose errors since. One was a 70-year-old man who was supposed to get 10mg of lisinopril - got a 40mg bottle. The system screamed. He’s alive today. No drama. Just a beep and a saved life. Worth every penny.
Let me tell you about the time I almost gave a patient warfarin instead of rivaroxaban. I was tired. My brain was on autopilot. The scanner went off. Red. Loud. I froze. I looked at the bottle. It was the right drug. But the strength? 5mg instead of 20mg. I didn’t catch it. The machine did. I cried after my shift. Not because I was scared - because I realized how fragile this all is. And how lucky we are that someone built this.
Ah yes, the classic 'technology fixes everything' narrative. Next they'll scan your soul to make sure you're not a bad person. Meanwhile, in Canada, we just have pharmacists who talk to patients. You know, like humans. But sure, let's keep pretending a barcode is a moral compass.
The data is clear. BCMA reduces preventable errors by over 90%. The only question is why more community pharmacies haven't adopted it. Cost is a factor. But so is inertia. And complacency. The silence after the alarm doesn't sound - that’s the sound of safety.
I work in a small pharmacy. We just got our scanner last month. It’s been a game changer. Even if it’s just one error caught, it’s worth it. We’re not saving the world - but we’re saving one person at a time. And that’s enough.