Cervical Myelopathy: Recognizing Spinal Stenosis Symptoms and When Surgery Is Needed

What Is Cervical Myelopathy?
Cervical myelopathy is a neurological condition caused by compression of the spinal cord in the neck. It’s not just a stiff neck or sore muscles-it’s when the spinal cord itself is being squeezed, often by narrowing of the spinal canal, known as cervical spinal stenosis. This compression doesn’t just cause pain. It interferes with the signals traveling between your brain and body, leading to real, measurable changes in how you move and feel.
Most cases-about 75%-are called cervical spondylotic myelopathy (CSM), which happens because of age-related wear and tear. Over time, discs dry out, bones grow spurs, ligaments thicken, and the space around your spinal cord shrinks. By age 70, nearly 1 in 10 people show signs of this condition, though not everyone has symptoms.
How Do You Know If It’s More Than Just a Stiff Neck?
The early signs of cervical myelopathy are subtle, and many people dismiss them as normal aging. But they’re not. You might notice your hands feel clumsy-like you’re dropping things, struggling to button shirts, or having trouble turning keys. These aren’t just "bad days." They’re red flags.
Here’s what to watch for:
- Hand clumsiness: Difficulty with fine motor tasks, like typing, writing, or picking up small objects.
- Gait problems: Feeling unsteady on your feet, shuffling, or bumping into things.
- Increased reflexes: Your doctor might find your knee or ankle reflexes are overly active during an exam.
- Numbness or tingling: Often in your arms, hands, or fingers-sometimes spreading to your legs.
- Balance issues: Feeling like you’re going to fall, even on flat ground.
- Bladder changes: Urgency to urinate or trouble controlling it-this usually comes later.
These symptoms don’t come on overnight. For about 45% of people, they creep in slowly over 2 to 5 years. But 25% of patients see things worsen fast-within months. That’s why ignoring early signs can be dangerous.
Why Diagnosis Takes Time-and Why It Matters
Many patients see three or more doctors before getting the right diagnosis. On average, it takes over a year from when symptoms start to when they’re confirmed. That delay matters.
Diagnosis isn’t just about pain. It’s about neurological function. Your doctor will check your reflexes, muscle strength, sensation, and coordination. But the real answer comes from imaging. An MRI is the gold standard. It can show exactly where the spinal cord is compressed and whether there’s damage inside the cord itself-something X-rays and CT scans can’t reveal.
A normal spinal canal is about 17-18mm wide. When it drops below 13mm, it’s considered stenotic. Below 10mm? That’s severe. But here’s the catch: about 1 in 5 adults over 40 have stenosis on an MRI with no symptoms at all. That’s why doctors don’t just rely on images-they match them with your symptoms. If your MRI shows narrowing and you have neurological deficits, that’s cervical myelopathy.
Can You Treat It Without Surgery?
Yes-but only if it’s mild and not getting worse. For patients with a JOA score of 12-14 (on a 17-point scale), doctors may try conservative care: physical therapy, avoiding heavy lifting, anti-inflammatory meds, and activity changes.
But here’s the hard truth: only 28% of people improve with non-surgical treatment over two years. The rest-63%-get worse. That’s why most experts agree: if your symptoms are moderate to severe (JOA score below 12), or if they’re progressing, surgery is the only reliable way to stop further damage.
Waiting too long can lead to permanent nerve injury. Once the spinal cord is scarred or damaged beyond repair, even the best surgery won’t restore full function.
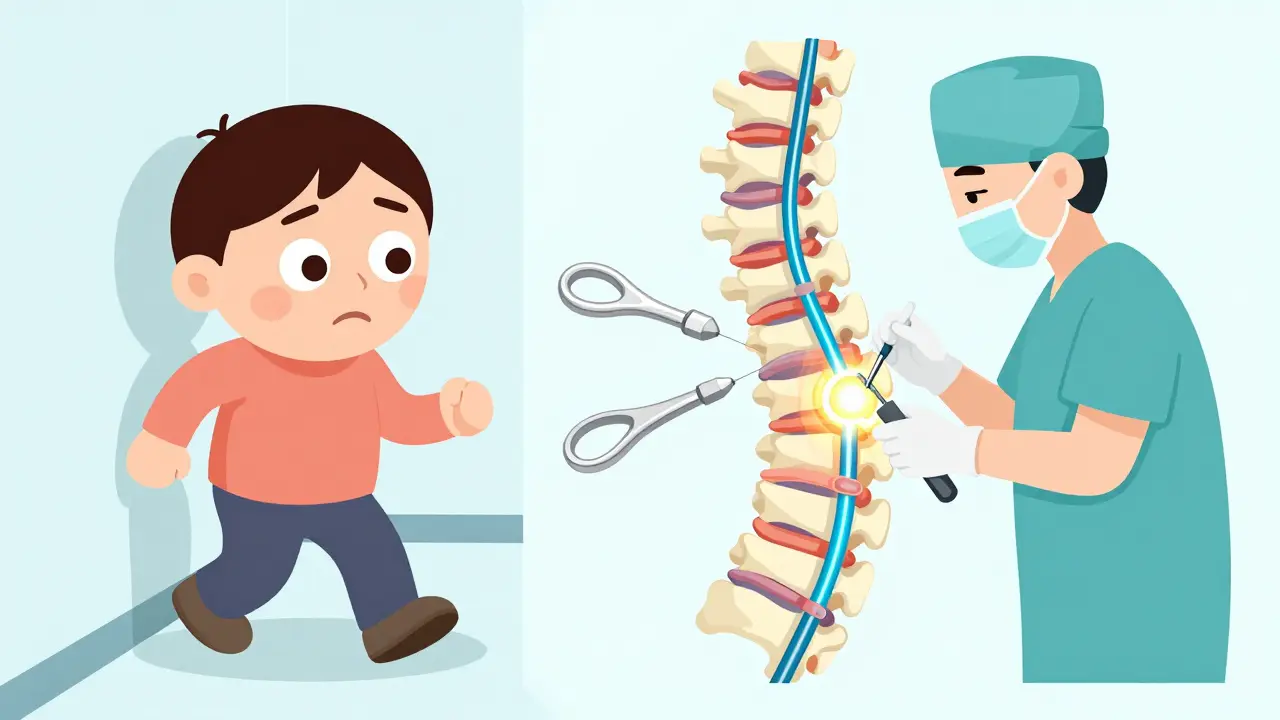
What Does Cervical Myelopathy Surgery Involve?
Surgery aims to take pressure off the spinal cord. There are two main approaches: front and back.
Anterior approach (from the front of the neck):
- Anterior Cervical Discectomy and Fusion (ACDF): Removes the damaged disc and fuses the vertebrae with a bone graft or implant. Best for one or two levels. Success rate: 85-90% for symptom relief.
- Cervical Disc Arthroplasty (artificial disc): Removes the disc but replaces it with a movable implant to preserve neck motion. Newer, FDA-approved for multiple levels since 2023. Early results show 81% success at 2 years.
Posterior approach (from the back of the neck):
- Laminectomy: Removes the back part of the vertebra to open up space. Often combined with fusion for stability.
- Laminoplasty: Hinges the back bone open like a door instead of removing it. Better for multiple levels, less neck pain afterward.
Choosing the right one depends on how many levels are affected, your spine’s alignment, and your overall health. Surgeons who perform more than 50 cervical procedures a year have 32% fewer complications.
What to Expect After Surgery
Most people go home in 1-3 days. Recovery isn’t quick. It takes 3 to 6 months to feel normal again. You’ll need physical therapy for 8-12 weeks to rebuild strength and relearn balance.
Here’s what patients commonly report:
- Positive outcomes: 82% see better hand function. 70-85% experience neurological improvement overall.
- Limitations: Only 65% regain normal walking ability. About 28% still need a cane or walker.
- Side effects: 35% have lingering neck pain after ACDF. 22% have trouble swallowing temporarily. 18% develop chronic neck pain after posterior surgery.
One of the biggest factors in success? Timing. Patients who have surgery within 6 months of symptoms start improving 37% faster than those who wait over a year. Delaying surgery by just one month can reduce recovery potential by 3%.

When Is Surgery Not the Answer?
Surgery isn’t risk-free. About 4-6% of patients face major complications: nerve injury, infection, or worsening symptoms. A rare but feared issue is C5 palsy-weakness in the shoulder or arm after surgery. The risk is higher if you have severe stenosis or other health problems.
Some people are better off not operating. If your symptoms are mild, stable, and you’re not declining, your doctor might suggest monitoring. If you’re over 80 with multiple health issues, the risks might outweigh the benefits.
And here’s a growing concern: up to 20% of cervical spine surgeries today might be unnecessary. Without clear signs of spinal cord damage, surgery won’t help-and could hurt.
What’s New in Treatment?
The field is evolving fast. In 2023, the FDA approved the first artificial disc for 2-3 level disease. Minimally invasive techniques now cut blood loss by 65% and shorten hospital stays. Researchers are even testing drugs like riluzole during surgery to protect nerves and boost recovery.
Future tools include robotic-assisted surgery and genetic testing to predict how fast degeneration will progress. Some people carry gene variants that make them more prone to rapid spinal cord damage. That could one day help doctors decide exactly when to operate-for you, not just for the average patient.
What Should You Do If You Suspect Cervical Myelopathy?
If you’re experiencing hand clumsiness, balance problems, or unexplained numbness in your arms or legs, don’t wait. See a spine specialist within 2-4 weeks. Get an MRI. Don’t settle for X-rays alone-they won’t show spinal cord damage.
Prepare for your appointment with notes:
- When did symptoms start?
- What tasks are harder now?
- Have you fallen more often?
- Do you have trouble with bladder control?
Stop smoking if you do-it cuts fusion success rates in half. Control your blood sugar if you’re diabetic. Get your physical therapy started early, even before surgery.
Remember: this isn’t a condition that gets better on its own. The longer you wait, the less likely you are to recover fully. But if caught early and treated right, most people go back to living their lives-just without the numbness, the falls, or the fear.
Can cervical myelopathy be cured?
Cervical myelopathy can’t always be fully "cured," but it can be effectively stopped and reversed in many cases. Surgery halts progression and often improves function-especially if done early. About 70-85% of patients see neurological improvement after surgery. However, if the spinal cord has been damaged for a long time, some deficits may remain permanent. Early treatment is key to maximizing recovery.
Is cervical myelopathy the same as spinal stenosis?
No. Spinal stenosis means the spinal canal is narrowed. Cervical myelopathy means that narrowing is actually damaging the spinal cord and causing neurological symptoms. You can have stenosis without myelopathy-many people do. But if you have myelopathy, you definitely have stenosis. The difference is whether your nerves are being injured.
How fast does cervical myelopathy progress?
Progression varies. About 45% of people get worse slowly over 2-5 years. 25% decline rapidly within 6-12 months. The rest may stabilize. But even if it seems slow, it doesn’t stop on its own. Without treatment, 20-60% will experience significant neurological decline over time. Early intervention prevents irreversible damage.
Can physical therapy cure cervical myelopathy?
Physical therapy alone cannot cure cervical myelopathy. It can help manage symptoms, improve strength, and maintain mobility-but it won’t relieve spinal cord compression. For mild cases with stable symptoms, therapy may delay surgery. But if symptoms are worsening, therapy won’t stop the damage. Surgery is the only way to remove the pressure on the spinal cord.
What are the risks of cervical spine surgery?
Risks include infection, bleeding, nerve injury, and failure to improve. Specific complications include C5 nerve palsy (shoulder weakness), difficulty swallowing (especially after anterior surgery), and chronic neck pain. About 4-6% of patients have major complications. Revision surgery is needed in 10% of cases over 10 years. Choosing an experienced surgeon and getting surgery early reduces these risks significantly.
How do I know if I need surgery?
You likely need surgery if you have moderate to severe symptoms (like hand clumsiness, gait instability, or bladder issues) and imaging confirms spinal cord compression. A JOA score below 12, or any sign of worsening over time, strongly indicates surgery is needed. If your symptoms are mild and stable, your doctor may monitor you. But if they’re getting worse, waiting is risky. Don’t wait for paralysis to decide.

14 Comments
I used to think my clumsiness was just getting older. Then I dropped my coffee mug three times in one morning and realized something was off. Turns out, it wasn't laziness-it was my spinal cord screaming for help. This post hit me right in the feels. Don't ignore the small things. Your body talks before it yells.
This is all Big Pharma propaganda. Spinal stenosis is caused by 5G towers and fluoride in the water. They want you to believe you need surgery so they can charge you $50,000 for a screw and a bone graft. Look up the real studies-none of this is proven. Trust your intuition, not the medical-industrial complex.
I had ACDF last year and honestly? Life-changing. 🙌 I couldn't button my shirts before. Now I'm back to knitting and playing guitar. It took 4 months to feel normal, but the pain was worth it. Don't wait until you're falling down stairs. Your future self will thank you.
Oh wow, so we're just supposed to trust the MRI like it's a crystal ball? And the JOA score? That's a fancy way of saying 'guess how bad you are.' Meanwhile, my cousin got surgery and now his left arm is basically a dead weight. You're telling me that's the best-case scenario?
I'm from India and we don't have access to MRIs like this. My dad had symptoms for 3 years before someone even mentioned spinal stenosis. We just did yoga and prayed. He's okay now, but I wish we knew sooner. This info is gold-please share it with people who can't afford specialists.
The statistical claims in this article are methodologically unsound. The 82% improvement rate for hand function is likely selection-biased, as it excludes patients who declined surgery or were excluded due to comorbidities. Furthermore, the 3% reduction in recovery potential per month is not derived from a longitudinal cohort study with proper controls. This is alarmist pseudoscience dressed as medical advice.
I've seen three patients with C5 palsy after laminoplasty. All were healthy, active men under 60. One never regained full deltoid strength. Surgery isn't a cure-it's a gamble. I don't push it unless the patient is losing bladder control. Then it's no longer a choice. Just... don't rush.
The fact that 1 in 5 adults over 40 have stenosis on MRI with zero symptoms? That’s wild. It’s like having a ticking time bomb in your neck that doesn’t even tick. I think we’re overmedicalizing aging. If you’re not falling, not numb, not losing grip-maybe just live your life. The spine isn’t a Lego set that needs fixing.
Americans and their surgeries. We had a man in London with the same symptoms who just did physio and changed his posture. He’s fine now. No metal in his neck. No hospital stay. Just common sense. You don’t need a robot to fix what a good chair and a walk can fix.
I work with elderly patients and let me tell you-this post is a godsend. One lady, 78, thought she was just clumsy. Turns out she was losing spinal cord function. We got her an MRI, she had surgery, and now she’s dancing at her granddaughter’s wedding. It’s not magic. It’s timing. Don’t wait for the cane. Don’t wait for the fall. Don’t wait for the tears. Just go. Your spine won’t wait for you to be ready.
I had this. I waited. I thought it was just carpal tunnel. Then I couldn’t hold my phone. Then I fell in the shower. Then I cried in the ER because I couldn’t feel my toes. Surgery saved me. But the worst part? The 6 months of PT where I had to relearn how to walk like a newborn deer. Don’t be me. Don’t wait until your body is a broken toy.
I am from Nigeria, and we have limited access to advanced neuroimaging. My brother had symptoms for four years before he was diagnosed. He is now partially paralyzed. This information is not just medical-it is a lifeline. I have translated this into pidgin English and shared it with three community health centers. Thank you for writing this with clarity and compassion.
As a retired IPS officer, I've seen too many people ignore early signs because they fear surgery. But let me tell you-pain is temporary. Paralysis is forever. This isn't about fear. It's about responsibility. If you're reading this and noticing hand clumsiness, don't wait for your doctor to say something. Go. Get the MRI. Take control. Your dignity depends on it.
My mom had this. She didn't want surgery. We pushed. She got it. Now she plays with her grandkids again. But I'll be honest-I cried for three days after the surgery. Not because she was in pain, but because I realized how close we came to losing her independence. This isn't just about the spine. It's about keeping the people you love alive in their bodies.