Clomiphene and Endometriosis: Can It Help You Conceive?

If you have endometriosis and are trying to get pregnant, you’ve probably heard about clomiphene. It’s one of the most common fertility drugs out there-but does it actually work when endometriosis is in the picture? The short answer: sometimes. But it’s not a magic fix, and it doesn’t help everyone.
What is clomiphene, really?
Clomiphene citrate, often sold under the brand name Clomid, is a pill that tricks your body into thinking estrogen levels are low. That triggers your brain to release more follicle-stimulating hormone (FSH) and luteinizing hormone (LH), which then push your ovaries to produce and release an egg. It’s used mostly for women who don’t ovulate regularly, like those with PCOS.
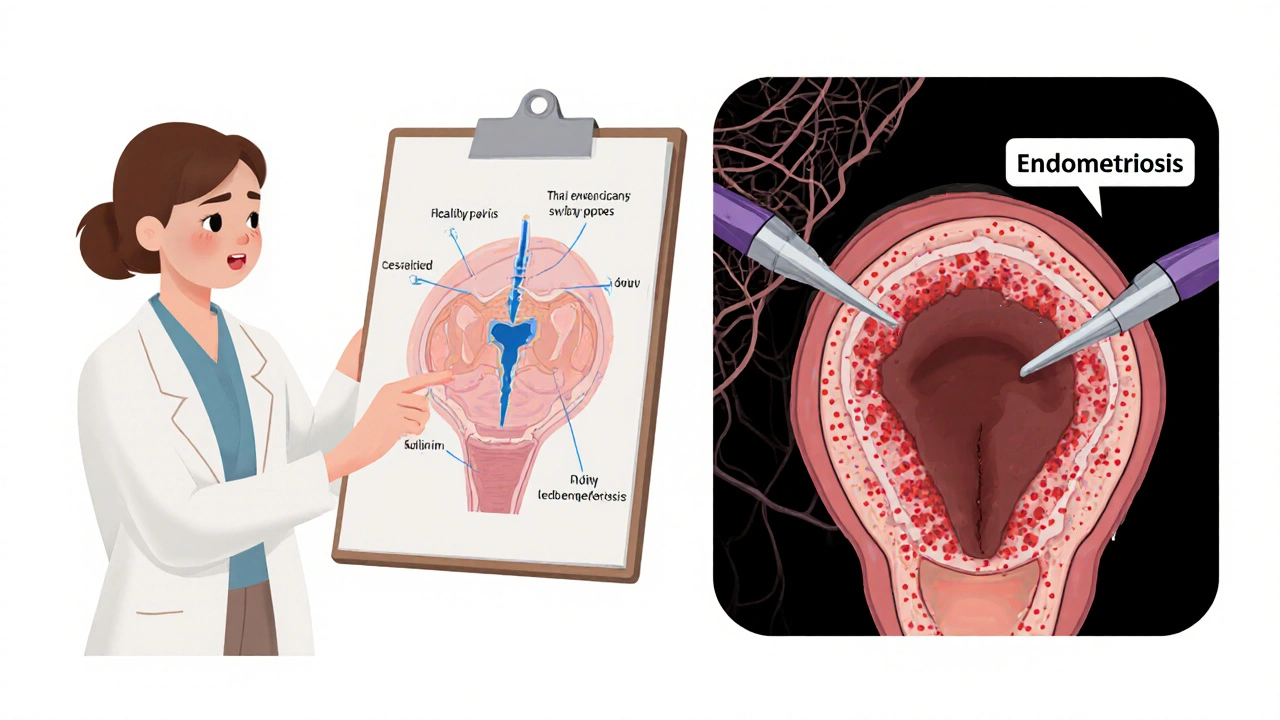
But endometriosis isn’t about lack of ovulation. It’s about tissue that acts like uterine lining growing outside the uterus-on the ovaries, fallopian tubes, bowel, or pelvic lining. This tissue bleeds and scars with each cycle, causing pain and sometimes blocking the path sperm or eggs need to meet.
So while clomiphene can get you ovulating, it doesn’t touch the scar tissue, inflammation, or blocked tubes that endometriosis causes. That’s the big gap.
Does clomiphene improve pregnancy rates in endometriosis?
Research shows mixed results. A 2021 study in the Journal of Reproductive Medicine followed 327 women with mild to moderate endometriosis who tried clomiphene for six cycles. About 28% got pregnant. That’s higher than the 10-15% natural conception rate for women with endometriosis, but lower than the 40-50% success rate seen with IVF.
Another study from 2023, published in Fertility and Sterility, found that clomiphene worked best for women with stage I or II endometriosis-mild cases with minimal scarring. For stage III or IV, where tubes are blocked or ovaries are damaged, clomiphene barely moved the needle. In those cases, doctors often skip straight to IVF.
Here’s the thing: clomiphene doesn’t fix the underlying problem. It just tries to force ovulation through a system already struggling with inflammation and physical barriers.
Who might benefit from clomiphene with endometriosis?
You might be a good candidate if:
- You have mild endometriosis (Stage I or II), confirmed by laparoscopy
- You ovulate on your own but inconsistently
- Your partner has normal sperm counts
- Your fallopian tubes are open (confirmed by HSG test)
- You’re under 35 and haven’t been trying for more than 12 months
For these women, clomiphene can be a low-cost, low-risk first step. It’s cheaper than IUI or IVF, doesn’t require injections, and can be started right away.
But if you have severe pain, blocked tubes, or ovarian cysts from endometriosis (endometriomas), clomiphene alone won’t cut it. You’ll likely need surgery first-or skip to IVF.
What are the downsides?
Clomiphene isn’t harmless. Common side effects include hot flashes, mood swings, headaches, and bloating. About 10% of women report blurred vision, which should stop you from driving or operating machinery.
It also thickens cervical mucus, making it harder for sperm to swim through. And it can thin the uterine lining-exactly the opposite of what you want when implantation is already tough due to endometriosis-related inflammation.
There’s also a 5-8% chance of twins with clomiphene. That’s higher than natural conception, but lower than with injectable fertility drugs. For women with endometriosis, multiples can mean higher risk of preterm birth and complications, especially if you’ve had pelvic surgery before.
And here’s something rarely talked about: clomiphene can make endometriosis symptoms worse for some women. The higher estrogen levels from stimulated ovulation may feed the misplaced tissue, increasing pain and inflammation. One 2022 patient survey found that 37% of women with endometriosis reported worse pelvic pain while on clomiphene.
What do doctors recommend instead?
For women with endometriosis, the most effective path to pregnancy usually involves a combination of approaches:
- Minimally invasive surgery: Laparoscopic removal of endometrial lesions can improve fertility, especially in mild to moderate cases. Many women conceive naturally within 6-12 months after surgery.
- IUI with gonadotropins: Instead of clomiphene, injectable hormones like FSH can produce more eggs with less impact on cervical mucus and uterine lining. IUI places sperm directly into the uterus, bypassing cervical issues.
- IVF: The gold standard for moderate to severe endometriosis. IVF bypasses blocked tubes and allows embryos to be transferred directly into the uterus. Success rates are 40-60% per cycle for women under 35 with endometriosis.
- Hormonal suppression before IVF: Some clinics give GnRH agonists (like Lupron) for 2-3 months before IVF to quiet endometriosis activity. This can improve implantation rates.
Clomiphene has its place-but it’s not the first-line treatment for endometriosis-related infertility. Most fertility specialists now recommend starting with surgery or IUI, especially if you’re over 30 or have been trying for over a year.
What should you do if you’re considering clomiphene?
Don’t start without a full fertility workup. Ask your doctor for:
- A hysterosalpingogram (HSG) to check if your tubes are open
- An AMH blood test to measure ovarian reserve
- An ultrasound to look for endometriomas or ovarian damage
- A laparoscopy if you have severe pain or haven’t had confirmation of stage
If your tubes are blocked or your ovarian reserve is low, clomiphene won’t help. If you’re over 35, time is critical-waiting for 6 cycles of clomiphene could cost you your best chance.
Also, track your cycle closely. Use ovulation predictor kits and basal body temperature charts. If you’re ovulating but still not getting pregnant after three cycles, it’s time to reassess.
Real stories: What worked for others
Jamila, 32, had stage II endometriosis and irregular cycles. She tried clomiphene for four months. Got pregnant on the fifth cycle. But she also had surgery six months before starting clomiphene-so her tubes were clear and the lesions were removed.
Tasha, 36, had stage IV endometriosis and two failed IUIs. Her doctor said clomiphene wouldn’t help. She went straight to IVF. Got pregnant on the first try. She says, "I wish I’d skipped the pills and gone to IVF sooner. The emotional toll of waiting was worse than the shots."
Maya, 29, took clomiphene for six cycles with no success. Her pain got worse. She stopped, got a laparoscopy, found deep infiltrating endometriosis on her bowel, had surgery, and got pregnant naturally within 8 months.
There’s no one-size-fits-all. But the common thread? Successful pregnancies came after proper diagnosis and targeted treatment-not just ovulation induction.
Bottom line
Clomiphene can help some women with mild endometriosis conceive-but only if the rest of their fertility picture is intact. It doesn’t fix scarring, inflammation, or blocked tubes. It doesn’t reduce pain. And it might even make symptoms worse.
If you have endometriosis and are trying to get pregnant, don’t assume clomiphene is your best bet. Talk to a reproductive endocrinologist. Get the full testing. Understand your stage. Know your options.
For many, surgery or IVF is the faster, more reliable path. Clomiphene might be a stepping stone-but it shouldn’t be the only one you try.
Can clomiphene make endometriosis worse?
Yes, for some women. Clomiphene increases estrogen levels, which can stimulate endometrial tissue outside the uterus, leading to more inflammation and pain. Studies show about 1 in 3 women with endometriosis report worsened symptoms while taking it. If your pain increases, talk to your doctor about stopping or switching treatments.
Is clomiphene safe if I’ve had endometriosis surgery?
It can be, especially if the surgery cleared blocked tubes and removed visible lesions. Many doctors recommend trying clomiphene or IUI for 3-6 cycles after surgery, especially if you’re under 35. But if you don’t conceive in that window, move on to IVF-waiting longer reduces your chances.
How long should I try clomiphene before switching?
Most fertility specialists recommend no more than six cycles of clomiphene. After that, the chances of pregnancy drop sharply, and the risk of side effects increases. If you haven’t conceived by cycle six, it’s time to consider IUI or IVF, especially with endometriosis.
Can I take clomiphene with other endometriosis medications?
Generally, no. Hormonal treatments like birth control pills, GnRH agonists, or progestins suppress ovulation and are meant to stop endometriosis growth. Taking clomiphene while on these drugs cancels out their effect and can cause unpredictable hormone spikes. Always talk to your doctor before combining treatments.
Does clomiphene work better than letrozole for endometriosis?
Letrozole, a breast cancer drug used off-label for fertility, often outperforms clomiphene in women with endometriosis. It doesn’t thicken cervical mucus or thin the uterine lining as much, and studies show slightly higher pregnancy rates. Many clinics now use letrozole as first-line for endometriosis-related infertility, especially in women over 30.

10 Comments
clomiphene made my pain WORSE like WHOA. i stopped after 2 cycles and just went straight to ivf. best decision ever. no more crying in the bathroom during ovulation. 🤍
The assertion that clomiphene is a viable first-line agent for endometriosis-associated infertility is not merely misguided-it is clinically indefensible. The pharmacological profile of clomiphene citrate exacerbates estrogen-dependent pathology, and its impact on cervical mucus and endometrial receptivity is demonstrably deleterious. To recommend it without laparoscopic confirmation of tubal patency and lesion burden is malpractice masquerading as advice.
Hey, I get why people are skeptical of clomiphene, but if you’ve got mild endo and your tubes are clear, it’s not the devil. I was on it for 3 cycles, got pregnant on the 4th. Didn’t have surgery first, but I did track my temps religiously and used OPKs. Also, my doc gave me a low dose-50mg, not 100mg. Big difference. And yes, I had hot flashes, but nothing like the IVF shots later. It’s not magic, but it’s not useless either.
Let’s be real-clomiphene is just a band-aid on a hemorrhage. The real issue is the inflammatory cascade driven by ectopic endometrial implants. Clomiphene doesn’t modulate IL-6, TNF-alpha, or VEGF expression-it merely induces anovulatory surges in a dysregulated HPO axis. Meanwhile, letrozole suppresses aromatase, reduces peritoneal fluid estrogen, and improves endometrial thickness. Why are we still clinging to 1960s pharmacology when we have 2020s evidence? The literature is unequivocal: letrozole > clomiphene for endometriosis. Period.
Just wanted to say THANK YOU for mentioning letrozole!! I was on clomiphene for 5 cycles and felt like a zombie. Switched to letrozole-same cost, way fewer side effects, and I got pregnant on cycle 2. Also, no more blurry vision or mood swings that made me yell at my cat. 🐱💕
Look, I’ve been through this. I had stage III endometriosis, blocked tubes, and a 37% AMH. I tried clomiphene because I was scared of IVF costs and didn’t think I’d qualify. Spoiler: I didn’t get pregnant. I cried. I felt broken. Then I found a clinic that offered payment plans and did a mini-IVF with Lupron prep. Got pregnant on the first try. The emotional toll of waiting? It’s real. The physical toll of clomiphene? Even worse. You don’t have to suffer through six cycles of false hope. There’s a path forward-and it doesn’t involve hoping your body fixes itself. You’re not failing if you skip to IVF. You’re being smart.
I had clomiphene after surgery and it worked-but only because my surgeon removed every visible lesion and my tubes were confirmed open. I was 28, no other issues. Three cycles, then pregnant. But I know so many who wasted a year on it. If you’re over 30, don’t wait. Get the HSG. Get the AMH. Get the ultrasound. Don’t let anyone tell you it’s ‘too early’ to go to IVF. Time is your enemy, not your ally.
Wait so if clomiphene makes endo pain worse… why do doctors still prescribe it? I feel like this whole thing is just a giant game of ‘try this, if it fails, try this, if it fails, try this’ and nobody ever says ‘hey, maybe skip to the thing that actually works.’
Thank you for sharing such a comprehensive overview. I appreciate the nuance-especially the emphasis on individualized treatment. For those of us navigating endometriosis-related infertility, the pressure to ‘just try something’ can be overwhelming. It’s reassuring to see evidence-based guidance that acknowledges the complexity of our condition. I hope more clinicians adopt this approach.
Clomiphene is a relic. Letrozole is better. IVF is faster. Surgery is necessary if you have adhesions. Stop wasting time. Your ovaries don’t care about your hopes. They care about your AMH and your age. Get tested. Get real. Move on.