Duloxetine and Liver Health: What You Need to Know About Hepatotoxicity Risk

Duloxetine Liver Risk Calculator
This calculator estimates your risk of elevated liver enzymes while taking duloxetine based on key health factors. It is not a medical diagnosis and should be used with professional medical advice.
Recommendations:
When you start taking duloxetine - whether for depression, anxiety, or chronic pain - most people assume the biggest concerns are side effects like nausea, dizziness, or sleep changes. But there’s a quieter, more serious risk that doesn’t get enough attention: duloxetine can harm your liver. It’s rare, but when it happens, it can be severe. And unlike some side effects that show up right away, liver damage often creeps in slowly, sometimes after weeks or months of taking the drug without warning.
Why Duloxetine Can Affect Your Liver
Duloxetine, sold under the brand name Cymbalta, is a serotonin-norepinephrine reuptake inhibitor (SNRI). It works well for mood disorders and nerve pain, but your body breaks it down using liver enzymes - mainly CYP1A2 and CYP2D6. Sometimes, this process creates small toxic byproducts that can damage liver cells. This isn’t an allergy or immune reaction; it’s a direct chemical effect on the liver tissue. The risk isn’t the same for everyone. People with existing liver disease, heavy alcohol use, or obesity are at higher risk. But here’s the catch: even healthy people with no history of liver problems can develop liver injury. A 2011 study from Korea found three cases of severe liver damage in Asian patients who drank little to no alcohol and had no prior liver conditions. That’s why blanket assumptions like “I’m young and healthy, so I’m fine” can be dangerous.How Common Is Liver Damage from Duloxetine?
Most people won’t have issues. But the numbers matter. Clinical trials show that about 1-2% of people taking duloxetine (60 mg daily) will have elevated liver enzymes - a sign the liver is under stress. In about 0.6% of cases, those enzyme levels rise more than three times the normal upper limit. That’s the red flag doctors watch for. Severe cases - where liver damage requires hospitalization - are rare: about 1 in 10,000 patients, based on FDA data from 2015 to 2020. But when it happens, it’s serious. There are documented cases of patients developing jaundice (yellow skin), dark urine, and abdominal pain after just 45 days on the drug. One patient’s ALT level hit 789 U/L - nearly 20 times the normal limit. They needed hospital care and three months to recover.When Does Liver Damage Show Up?
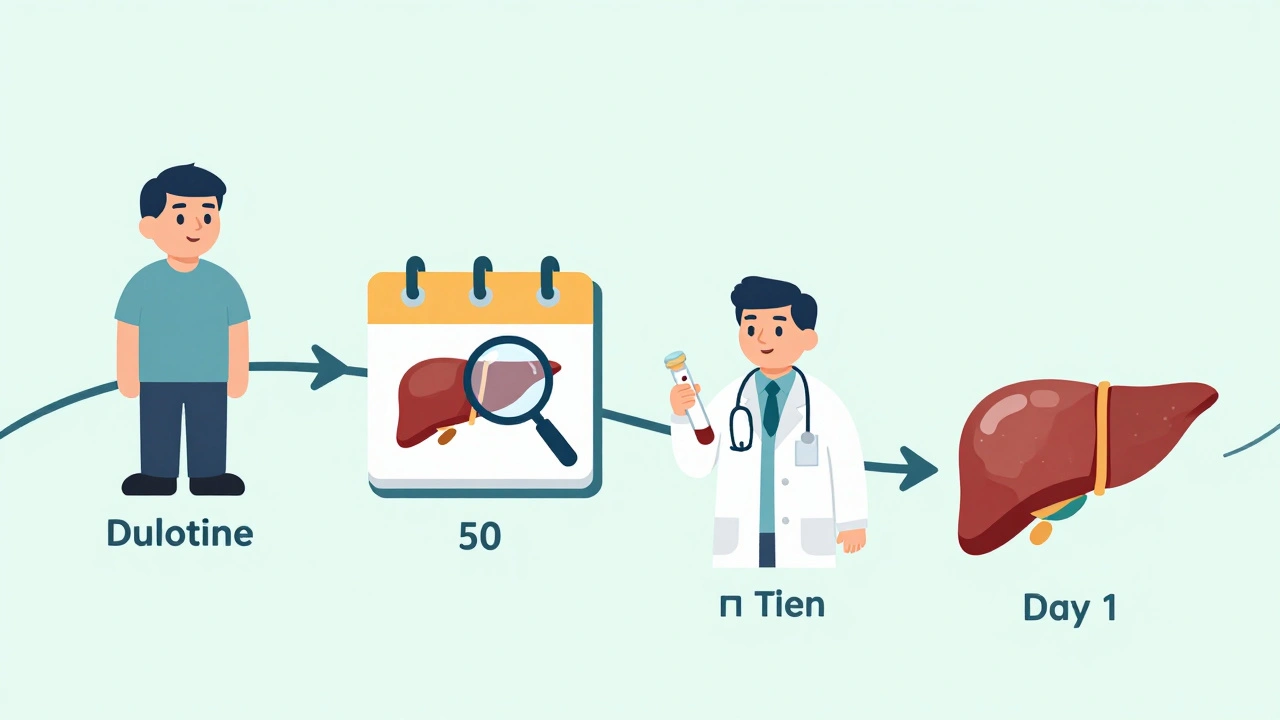
Timing is critical. Most cases of duloxetine-related liver injury appear between 35 and 62 days after starting the medication. The median time? Around 50 days. That’s not a coincidence. It’s the window when your body has had enough time to build up the drug and its metabolites to a level that starts stressing liver cells. This is why the first few weeks aren’t the only time to pay attention. Many patients and even some doctors think if you’ve made it past the first month without side effects, you’re in the clear. But for liver damage, the real danger zone is weeks 5 to 9. That’s when you need to be extra alert - not just for how you feel, but for lab results.What Symptoms Should You Watch For?
You won’t always feel sick at first. Liver damage often starts silently. But as it progresses, you might notice:- Dark urine (like tea or cola)
- Yellowing of the skin or eyes (jaundice)
- Unexplained fatigue or weakness
- Loss of appetite, nausea, or vomiting
- Itchy skin without rash
- Light-colored or clay-colored stools
- Pain or swelling in the upper right abdomen
Who’s at Highest Risk?
Some people are more vulnerable than others. The main risk factors include:- Obesity (BMI 30 or higher)
- Diabetes
- Chronic alcohol use (more than 14 drinks per week for men, 7 for women)
- Already having liver disease, including fatty liver
- Taking other medications that affect the liver - like statins, NSAIDs, or certain antibiotics
- Being a poor metabolizer of CYP2D6 (a genetic factor)
How Doctors Should Monitor You
There’s no single rule everyone follows - but the best practices are clear. The American Psychiatric Association and the American Association for the Study of Liver Diseases both recommend:- Baseline blood tests before you start duloxetine: ALT, AST, alkaline phosphatase, and bilirubin.
- Repeat testing at 8-12 weeks after starting, especially if you’re in a high-risk group.
- More frequent testing (every 4-6 weeks) if you’re on higher doses, have risk factors, or are taking other liver-affecting drugs.
What Happens If Your Liver Enzymes Go Up?
If your blood test shows ALT or AST levels more than three times the upper limit of normal:- Don’t panic - but don’t ignore it.
- Your doctor should repeat the test within 1-2 weeks to confirm.
- If levels stay high or climb higher, they’ll likely stop duloxetine.
- If levels exceed five times the upper limit, or if you have symptoms, stopping the drug is urgent.
How Duloxetine Compares to Other Antidepressants
Not all antidepressants carry the same liver risk. Compared to SSRIs like sertraline or escitalopram, duloxetine has about a 1.8 times higher chance of causing significant ALT elevation. Venlafaxine, another SNRI, has a similar risk profile. Tricyclic antidepressants (like amitriptyline) are more likely to affect your heart rhythm, so they need ECG monitoring. Bupropion carries a seizure risk. Duloxetine’s main red flag? Your liver. That’s why it’s not a one-size-fits-all drug. If you’ve had liver trouble before, your doctor might choose something else.Real Patient Stories
Online forums are full of mixed experiences. One patient, ‘AnxietyWarrior42,’ developed jaundice and liver failure after 45 days on 60 mg duloxetine. Their ALT hit 789 U/L. They were hospitalized. Recovery took months. Another, ‘ChronicPainSurvivor,’ took 60 mg daily for five years. Their ALT hovered between 52 and 68 U/L - slightly above normal but never dangerous. They stayed on the drug with quarterly blood tests and felt fine. The difference? Monitoring. The first person had no baseline test. The second had regular check-ups. One was lucky. The other was careful.What’s Changing in 2025?
New guidelines are coming. The American College of Gastroenterology is expected to release updated recommendations by late 2024, and early drafts suggest all SNRIs should get baseline liver tests - not just duloxetine. The FDA is also reviewing its drug-induced liver injury guidelines, which could lead to more standardized monitoring rules across the board. Research into genetic testing is advancing too. A 2023 study found that people with a CYP2D6 poor metabolizer gene variant are 2.4 times more likely to develop liver injury on duloxetine. That test isn’t routine yet - but it might be soon.What You Should Do
If you’re taking duloxetine or thinking about it:- Ask your doctor for baseline liver tests before you start.
- Get a follow-up test at 8-12 weeks - even if you feel fine.
- Know the warning signs. Don’t brush off fatigue or dark urine.
- If you’re overweight, diabetic, or drink alcohol regularly, push for more frequent monitoring.
- Don’t stop the drug suddenly if you need to discontinue - work with your doctor on a slow taper to avoid withdrawal symptoms.
Can duloxetine cause permanent liver damage?
In rare cases, yes. Most people recover fully after stopping duloxetine, with liver enzymes returning to normal within weeks or months. But if liver injury is ignored and the drug is continued, it can lead to acute liver failure or chronic damage. This is why early detection through blood tests is critical.
Do I need blood tests if I’m healthy?
Yes. Even if you’re young and healthy, duloxetine can still affect your liver. About half of all reported cases occur in people with no known risk factors. Baseline testing is simple, inexpensive, and can catch problems before they become dangerous. Skipping it is like driving without checking your brakes.
Is it safe to take duloxetine with other medications?
It depends. Many common drugs - like statins, ibuprofen, certain antibiotics, and even some herbal supplements - can stress the liver. Taking them with duloxetine increases the risk of damage. Always tell your doctor about everything you’re taking, including vitamins and over-the-counter pills.
How long does it take for liver enzymes to return to normal after stopping duloxetine?
Most patients see improvement within 4-8 weeks after stopping. Full recovery can take up to 3-6 months. If enzymes haven’t improved after 3 months, further testing is needed to rule out other causes of liver damage.
Can I restart duloxetine if my liver enzymes returned to normal?
Generally, no. Once you’ve had duloxetine-induced liver injury, rechallenging (taking it again) carries a high risk of recurrence - often more severe. Most doctors recommend avoiding duloxetine and all SNRIs in the future. Alternative treatments like SSRIs or therapy-based approaches are safer options.
Are there natural ways to protect my liver while on duloxetine?
No supplement or herb has been proven to prevent duloxetine-related liver damage. Milk thistle, NAC, or vitamin E won’t shield your liver from the drug’s metabolic byproducts. The only proven protection is regular blood tests and avoiding alcohol. Trying to “detox” with supplements can be misleading - and dangerous if it makes you delay medical care.

10 Comments
Really appreciate this breakdown - most people don’t realize liver damage from duloxetine can sneak up after months. I’ve seen patients bounce back fully with early detection, but I’ve also seen the ones who ignored the dark urine and paid the price. Baseline labs aren’t optional. They’re your first line of defense.
And yes, even if you’re young, healthy, and drink green tea every morning - your liver doesn’t care about your Instagram bio. Test it anyway.
People today think medicine is just a Google search away. You take a pill because you feel ‘sad’ and expect your liver to handle it like a superhero. No. Your liver isn’t a vending machine. It’s an organ that works 24/7 while you binge Netflix and eat takeout. If you’re not getting bloodwork done, you’re not being responsible - you’re being reckless.
WHO IS ALLOWING THIS DRUG TO BE SOLD?! In India, we have real doctors who don’t just prescribe pills like candy - we have Ayurveda, we have yoga, we have discipline! And now you’re telling me some American pharma company is poisoning people with SNRIs because they didn’t do their homework?!
And don’t even get me started on ‘baseline tests’ - if your doctor doesn’t offer them, fire them! Find someone who actually cares! This isn’t 1990 anymore - we have labs, we have tech, we have COMMON SENSE!!
I was on duloxetine for 18 months for chronic back pain. My ALT was always normal, but I still got tested every 10 weeks like clockwork. My doctor said, ‘Better safe than sorry’ - and I’m glad I listened.
One time, my ALT spiked to 58 - just barely above normal. We paused the med for two weeks, retested, and it dropped back down. I restarted at 30mg. Still working fine two years later.
Monitoring isn’t paranoia. It’s precision medicine. And it works.
It is, without question, a matter of considerable clinical concern that the FDA does not mandate routine hepatic monitoring for SNRIs, particularly given the documented incidence of idiosyncratic hepatotoxicity. The absence of standardized protocols reflects a systemic failure in pharmacovigilance infrastructure - one that disproportionately impacts patients who lack access to specialist care.
Furthermore, the notion that ‘I’m healthy’ confers immunity is not merely misguided; it is an epistemological fallacy rooted in the commodification of health literacy.
Thank you for sharing this. I’ve been working with chronic pain patients for over a decade, and duloxetine has helped many - but only when used with caution.
Always check liver enzymes before starting. Always recheck at 8 weeks. Always ask about alcohol, supplements, and other meds.
And if your doctor says, ‘You’re fine, no need for blood work’ - walk out. Find someone who takes liver health seriously. Your future self will thank you.
Liver damage? From a depression pill? Wow. Next they’ll tell us oxygen causes lung cancer. This is just Big Pharma fearmongering to sell more tests. I’ve been on duloxetine for 7 years. My liver is fine. My doctor says I’m fine. End of story.
I’m from Mexico City and my abuela used to say ‘if your body feels off, listen to it’ - and she was right. I started duloxetine last year, felt tired for a while, thought it was stress… then I noticed my pee looked like cola. I went to the clinic, got tested, ALT was 120. Stopped the med. Three months later, back to normal.
Don’t wait until you’re yellow. Just check.
And no, milk thistle didn’t help. Just the test did.
They’re hiding something. Why do you think the FDA doesn’t require testing? Because they’re in bed with the drug companies. Look at the timeline - 50 days? That’s not random. That’s when the profit window closes and the liability window opens. They count on you to ignore the symptoms until it’s too late. Wake up.
And don’t even get me started on ‘genetic testing’ - they’re already planning to charge you $300 for a test they could’ve done for free in 2015. This is all about money. Not your liver.
Let me tell you something - in Nigeria, we don’t have access to these fancy blood tests. We take what we can get. My cousin took duloxetine for anxiety. Got jaundice. Was hospitalized. Came out with liver damage. No tests. No warnings. Just a prescription and a prayer.
So don’t talk to me about ‘baseline labs’ like it’s a luxury. For millions, it’s a myth. And that’s the real tragedy here.