Effective Sundowning Management for Alzheimer’s Dementia Caregivers

When a loved one with Alzheimer-type dementia a progressive brain disorder that erodes memory, judgment and behavior becomes unusually restless, confused, or fearful as the day winds down, many families label the episode "sundowning." This guide walks you through what triggers those evening spikes, how to shape the environment, which simple routines can calm the storm, and when medicines might be needed. By the end you’ll have a concrete plan you can start using tonight.
Key Takeaways
- Identify lighting, noise, and fatigue as common sundowning triggers.
- Establish a predictable evening routine that includes calming activities and reduced stimulation.
- Use non‑pharmacologic tools-like light therapy, aromatherapy, and sleep hygiene-before considering medication.
- Keep safety measures in place: low‑level nightlights, secured doors, and clear pathways.
- Don’t shoulder it alone; join support groups and know when to call a clinician.
What Is Sundowning?
Sundowning the pattern of increased confusion, agitation, and wandering that emerges in the late afternoon or early evening in people with dementia is not a myth-studies show up to 70% of Alzheimer’s patients experience it at some point. The term captures the "sunset" effect, where sensory overload, fatigue and disrupted circadian rhythms converge, making the person feel unsafe and over‑stimulated.
Why It Happens: Triggers and Underlying Factors
The brain changes of Alzheimer-type dementia reduce the ability to process visual and auditory cues, regulate sleep, and manage stress hormones lay the groundwork, but external factors often light the fuse.
- Lighting changes: Dimming natural light signals the brain that night is near, yet abrupt darkness can be disorienting.
- Noise spikes: Household activity, TV volume, or distant traffic become louder as background sounds fade.
- Fatigue: Accumulated mental effort throughout the day reduces coping capacity.
- Unmet needs: Hunger, thirst, pain, or the urge to use the bathroom may be hard to express.
- Medication timing: Some drugs wear off in the evening, while others stimulate rather than calm.
Practical Management Steps
Effective sundowning management blends environment tweaks, routine consistency, and targeted therapeutic tools.
1. Optimize Lighting and Visual Cues
Light therapy the use of bright, blue‑enriched light to reinforce daytime alertness and help reset circadian rhythms can be a game‑changer. Install a 10,000‑lux light box for 30 minutes after breakfast, or keep a full‑spectrum lamp on in the early evening. When the sun sets, switch to soft, warm bulbs (2700K) and use low‑level nightlights along hallways to prevent sudden darkness.
2. Establish a Calming Evening Routine
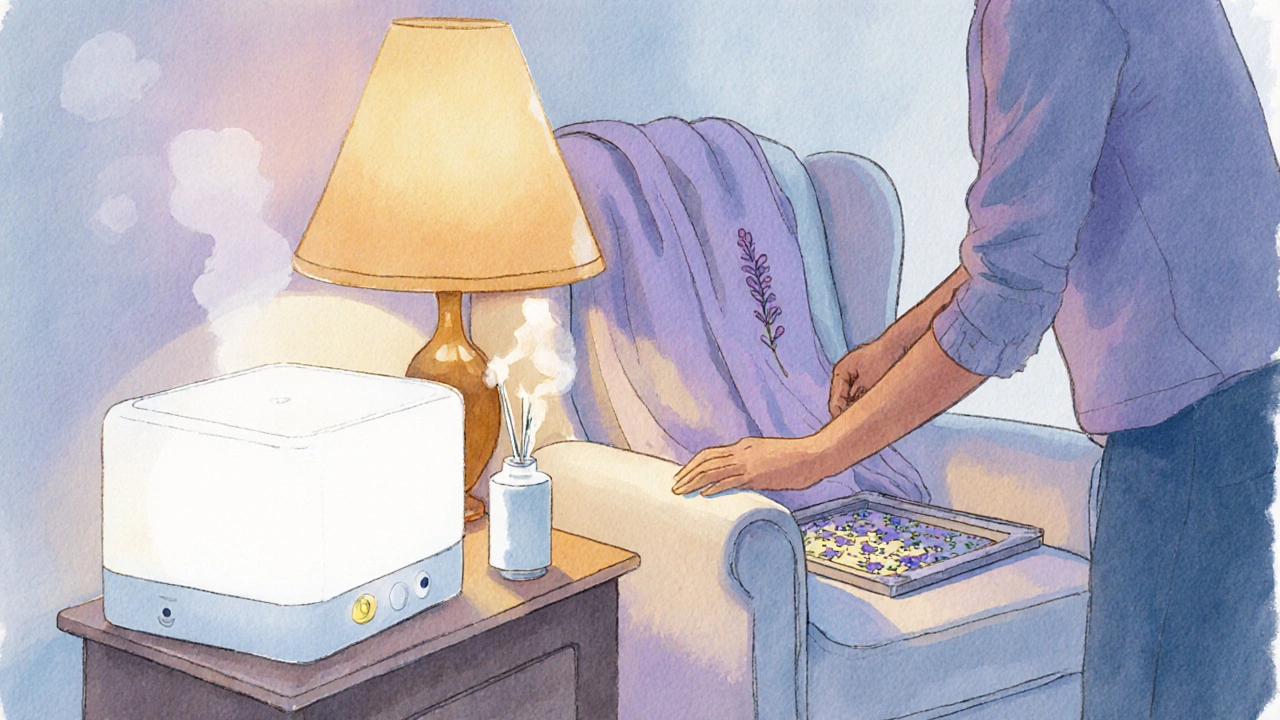
Predictability reduces anxiety. Follow the same sequence each night-light a scented candle, serve a light snack, play gentle music, then move to a favorite chair for a short conversation or simple puzzle. Aim to start winding down at least one hour before the usual bedtime.
3. Prioritize Sleep Hygiene
Sleep hygiene practices that promote uninterrupted, restorative sleep, such as consistent bedtime, limiting caffeine, and creating a quiet bedroom is essential. Keep the bedroom cool (around 65°F), block external light with blackout curtains, and avoid electronic screens after sunset.
4. Use Aromatherapy and Sensory Comfort
Lavender, rosemary or citrus essential oils diffused at low concentration can lower heart rate and calm the nervous system. Pair scent with a familiar plush blanket or a soft‑textured pillow to give a reassuring tactile cue.
5. Adjust the Physical Environment
Environmental modification changes to the home layout that reduce confusion, hazards, and overstimulation includes labeling doors with pictures, removing loose rugs, and placing a chair in high‑traffic areas for safe sitting.
6. Consider Medication Wisely
If non‑pharmacologic steps don’t keep agitation under control, a physician may prescribe low‑dose antipsychotics, melatonin, or cholinesterase inhibitors such as donepezil a medication that can modestly improve cognition and may reduce nighttime confusion. Always weigh benefits against side‑effects like increased falls or daytime sedation.
7. Employ Behavioral Therapy Techniques
Guided reminiscence-showing old photos or playing familiar songs-can anchor the person to a comfortable reality, reducing the urge to wander.
| Approach | Key Actions | Pros | Cons |
|---|---|---|---|
| Non‑Pharmacologic | Light therapy, routine, aromatherapy, sleep hygiene, environment tweaks | No drug side‑effects; enhances overall quality of life | Requires consistency; benefits may appear slowly |
| Pharmacologic | Low‑dose antipsychotics, melatonin, cholinesterase inhibitors (e.g., donepezil) | Can quickly reduce severe agitation | Risk of falls, sedation, metabolic issues; needs physician oversight |
Safety & Monitoring Tips
Even with a solid plan, safety remains paramount.
- Place nightlights near stairs and bathrooms.
- Lock exterior doors but keep a spare key within easy reach for emergencies.
- Use a medical alert bracelet if wandering is a risk.
- Document patterns: note time, trigger, response, and what helped. A simple spreadsheet can reveal trends for your doctor.

Supporting the Caregiver
Managing sundowning can be exhausting. Recognize your own limits-take a short break each evening, rotate duties with family members, and stay hydrated.
Joining online forums or local caregiver support groups peer gatherings where families share experiences and practical tips for dementia care provides emotional relief and fresh ideas. Professional respite services, even a few hours a week, can prevent burnout.
When to Seek Professional Help
Call a neurologist or geriatrician if:
- Agitation escalates to aggression or self‑harm.
- Falls or injuries occur more than once a month.
- Sleep deprivation begins to affect your health.
- Medications no longer control symptoms after a trial period.
A rapid assessment can adjust treatment plans, introduce new therapies, or suggest a short‑term hospice evaluation if end‑of‑life comfort becomes the focus.
Frequently Asked Questions
Why does sundowning start suddenly for some patients?
The brain’s internal clock (circadian rhythm) becomes fragmented as dementia progresses. Diminished light perception in the evening, combined with fatigue, triggers a surge of confusion and anxiety.
Can diet affect sundowning?
Yes. Heavy, spicy meals close to bedtime can cause discomfort and disrupt sleep. Opt for light protein (e.g., yogurt, boiled egg) and a small portion of complex carbs to keep blood sugar stable.
Is melatonin safe for dementia patients?
Low‑dose melatonin (0.5‑3mg) is often well‑tolerated and can help reset sleep cycles. Always discuss dosage with a doctor, especially if the patient is on other CNS‑active drugs.
How much light is needed for effective light therapy?
A box that delivers 10,000 lux at a distance of 12‑18 inches for 20‑30 minutes each morning is the standard protocol. Consistency matters more than occasional longer sessions.
What are signs that medication is needed?
When non‑drug strategies fail after two weeks, or when agitation leads to falls, aggression, or severe insomnia, a clinician may consider a short‑term antipsychotic or a cholinesterase inhibitor.

16 Comments
Honestly, most caregivers think they can wing it with a handful of tips, but sundowning isn’t a weekend project-it's a relentless, neon‑lit battle. The guide tries to be a Swiss‑army knife, yet it drops the ball on real‑world grit. If you’re not ready to turn your living room into a therapeutic sanctuary, you’ll just be adding to the chaos. Bottom line: read it, adapt it, and stop whining when the night gets rough.
First, thank you for putting together such a comprehensive overview; the depth of research shines through every section. I’d like to add that consistency is the hidden backbone of any successful sundowning strategy, and families should consider a visual schedule that spans the entire day, not just the evening. Aligning meals, medication, and light exposure with a predictable timeline reduces the cognitive load on the patient and gives the caregiver a reliable framework. In my experience, integrating gentle physical activity-like a 10‑minute walk after lunch-can significantly lower the evening agitation that often stems from pent‑up energy. It’s also worth noting that humidity levels around 45–50 % can improve comfort, especially for those who tend to feel “sticky” at night, which can exacerbate confusion. For lighting, consider using programmable smart bulbs that gradually dim over a 30‑minute window, mimicking a natural sunset; this gentle transition can be far more soothing than an abrupt switch. Aromatherapy should be introduced gradually; start with a few drops of lavender on a cotton ball placed near the bedside, and monitor any allergic reactions before scaling up. Regarding nutrition, a small protein‑rich snack-like a handful of nuts or a boiled egg-about an hour before bedtime can stabilize blood sugar and prevent nocturnal restlessness. If the caregiver feels overwhelmed, rotating duties on a 2‑hour shift schedule can provide much‑needed respite and prevent burnout. Also, keep a “red‑flag” journal that logs specific triggers, timestamps, and successful interventions; over weeks, patterns usually emerge that can be shared with the treating neurologist. When contemplating medications, always discuss the risk‑benefit ratio, especially with antipsychotics, and explore melatonin titration schedules before moving to more potent agents. Remember to involve the person with dementia in the process as much as possible; even simple choices like selecting the evening playlist can foster a sense of agency. Finally, community resources such as local Alzheimer’s support groups often have volunteer “night‑watch” programs that can provide peace of mind during high‑risk hours. By layering these practical nuances onto the solid foundation you’ve already laid, families can transform sundowning from a nightly nightmare into a manageable rhythm. Consistent reflection and adaptation will keep the plan relevant as the disease progresses.
The neurocognitive diurnality shift observed in late‑stage Alzheimer’s exemplifies a dysregulation of homeostatic set‑points wherein melatonin secretion trajectories become decoupled from photic entrainment resulting in circadian misalignment this exacerbates behavioral phenotypes such as agitation and wandering which are clinically operationalized as sundowning thereby necessitating multimodal interventions spanning phototherapy, chronobiology, and environmental ergonomics
The article provides a solid foundation; however, it could benefit from a more rigorous discussion of the evidence hierarchy supporting each intervention. A citation matrix would enhance its academic utility.
Oh, brilliant, another “quick fix” for the endless night‑time drama-because we all know dementia just needs a scented candle and a sprinkle of positivity, right? I suppose if we ignore the neurobiology and just chant “good vibes” the brain will magically reboot. Sure, let’s all pretend that a lavender aroma can erase years of synaptic loss. Maybe next you’ll suggest yoga for the hippocampus. It’s adorable how we reduce complex pathology to mood‑lighting, as if the poor soul could just “feel better.”
Light therapy works but you must be consistent it isn’t a one‑off miracle
If you think aromatherapy solves everything it’s just a scented distraction
Alas, the twilight of the mind looms, and even the most diligent caregiver may feel like a lone voyager on a stormy sea, yet the guide offers a lighthouse of hope that flickers yet does not wane.
I’ve tried the bedtime routine you suggested and it really helped my mom settle more quickly; the low‑level nightlights make a big difference.
Honestly, the “one‑hour before bed” rule is just another arbitrary clock‑watching habit that doesn’t respect personal rhythms.
We must remember that the person behind the disease deserves dignity; imposing strict schedules without consent feels like a subtle form of oppression, even if the intention is to prevent harm.
This whole sundowning thing is overhyped.
Great job compiling these tips! 🌟 Remember, self‑care is just as important-take a short walk, sip some tea, and recharge. You’ve got this! 💪
Interesting points-does anyone have data on how different cultures adjust lighting in elder homes? 🤔
Indeed, the interplay between circadian biology and environmental stimuli constitutes a delicate symphony, wherein each photon of light, each whisper of scent, and each whispered reassurance compose a harmonic convergence that may alleviate the tempest of sundowning; nevertheless, one must not overlook the intrinsic agency of the individual, whose lived narrative weaves through the fabric of these interventions, demanding respect, empathy, and a tailored approach; consequently, caregivers are urged to adopt a praxis that balances scientific rigor with compassionate flexibility, lest the mechanistic application of protocols become a sterile echo devoid of humanity.
Stick to the routine, keep the lights low, and remember you’re doing an amazing job.