Generic vs Brand Identification in Pharmacy Systems: Best Practices for Accurate Medication Dispensing

Why generic vs brand identification matters in pharmacy systems
Every day, pharmacists face a simple but critical question: should this prescription be filled with the brand name or the generic version? It’s not just about cost-it’s about safety, legality, and patient trust. The U.S. Food and Drug Administration (FDA) says generic drugs are identical to brand-name drugs in active ingredients, strength, dosage, and performance. But in real-world pharmacy systems, things get messy. A patient might get a different pill shape, color, or inactive ingredient. Systems that can’t tell the difference between a brand and a generic-or worse, confuse an authorized generic with a branded generic-put patients at risk.
From 2009 to 2019, generic drugs saved the U.S. healthcare system nearly $2 trillion. That’s huge. But those savings only work if the right drug gets to the right patient. If a system mislabels a generic as a brand-or fails to flag a narrow therapeutic index (NTI) drug like warfarin or levothyroxine-small errors can lead to serious harm. In 2021, the Institute for Safe Medication Practices reported 147 adverse events over 18 months just from inappropriate generic substitution of NTI drugs. That’s not a glitch. That’s a system failure.
How pharmacy systems actually tell generics apart
At the heart of every pharmacy system is the National Drug Code (NDC). It’s a unique 10- or 11-digit number assigned to every drug product-brand or generic. But the NDC alone isn’t enough. The real key is the FDA’s Therapeutic Equivalence (TE) code, found in the Orange Book. These two-letter codes tell you if a generic is interchangeable with the brand. An ‘AB’ code means it’s bioequivalent and substitutable. An ‘BX’ code? Don’t substitute. It’s not proven equivalent.
Systems like Epic, Cerner, and Rx30 pull this data directly from the FDA’s Orange Book, updated monthly. But here’s where it gets tricky: authorized generics. These are the exact same pills as the brand, just sold under a different label. They share the same NDC as the brand but are listed as generics in the system. If your pharmacy software doesn’t flag them correctly, a pharmacist might think they’re switching to a cheaper version when they’re actually giving the patient the same exact drug.
Then there are branded generics-drugs like Errin, Jolivette, or Sprintec. They’re approved through the ANDA process (like all generics), but they carry a brand name. A patient might recognize “Sprintec” and refuse to take “norgestimate/ethinyl estradiol,” even though they’re the same. Pharmacy systems need to show both names side by side, or patients will get confused-and may skip their meds.
What the best pharmacy systems do differently
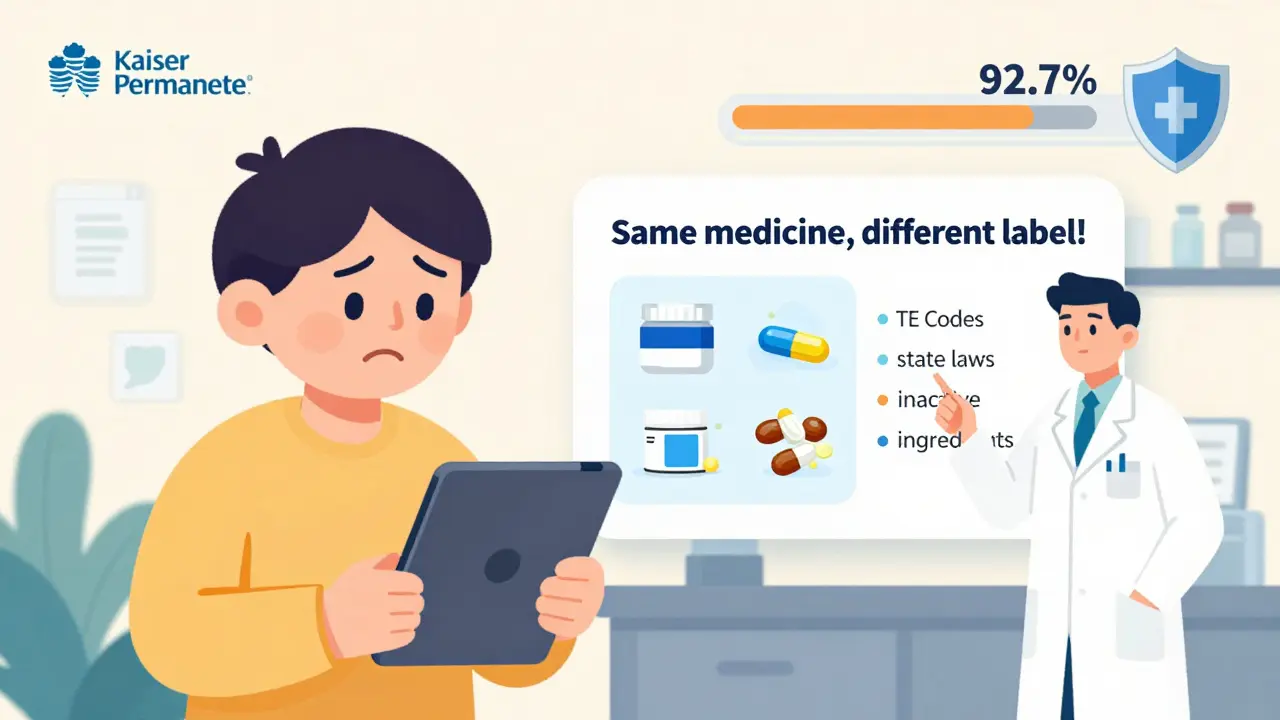
High-performing pharmacy systems don’t just list drugs-they guide decisions. Kaiser Permanente’s system defaults to generics unless there’s a clinical reason not to. That’s not just cost-saving-it’s safety-first design. When a prescriber writes “Lisinopril 10 mg,” the system doesn’t just show the brand. It shows all 17 approved generics, with TE codes and manufacturer info. It even highlights authorized generics with a special tag.
For NTI drugs, these systems don’t just warn-they lock. If someone tries to substitute warfarin, phenytoin, or levothyroxine, the system blocks the change unless the prescriber overrides it with a note. That’s not automation gone wrong. That’s smart design. In 2022, Kaiser’s system achieved a 92.7% generic dispensing rate without increasing adverse events. How? Because their system knew when to say no.
Another best practice: integration. The best systems don’t just use the Orange Book. They sync with DailyMed for inactive ingredient data and state-specific substitution laws. California requires pharmacists to document why they didn’t substitute. Texas doesn’t. Your system must know the difference-or you risk legal trouble.
Where systems fail-and why patients get confused
Despite all the tech, gaps remain. A 2023 Reddit thread from a Walgreens pharmacist revealed a common problem: their system listed 17 different lisinopril generics but didn’t say which ones were authorized. Patients were getting confused. They thought they were getting a “cheap knockoff” when they were actually getting the exact same drug as the brand.
Another blind spot: inactive ingredients. The FDA requires generics to match the brand in active ingredients and bioavailability-but not in fillers. A 2019 study in U.S. Pharmacist found 0.8% of patients switching from brand to generic antiepileptic drugs reported issues, likely due to differences in dyes or binders. Pharmacy systems rarely flag these. If a patient has a known allergy to a dye, or a gluten sensitivity, the system won’t know unless the prescriber manually adds a note.
And then there’s communication. A Consumer Reports survey found that 89% of patients were happy with generics-if they understood why they were switching. But only 63% were satisfied when the switch happened without explanation. That’s not a drug problem. That’s a communication failure. If your pharmacy system doesn’t have a built-in patient handout or digital popup explaining bioequivalence, you’re missing half the battle.
Training and protocols that actually work
Technology alone won’t fix this. People need training. ASHP recommends 8-10 hours of annual training for pharmacy staff on generic identification. That includes:
- How to read TE codes and NDCs
- Recognizing authorized vs. branded generics
- Understanding state substitution laws
- When to override system defaults
Humana’s system takes it further. It doesn’t just show generics-it suggests alternatives. When a prescriber writes a brand-name drug, the system pops up: “A generic version is available and FDA-approved. Would you like to switch?” The prescriber can accept, decline, or request a specific generic. Result? A 22% increase in generic use without a single safety incident.
For independent pharmacies, this might seem expensive. But the cost of getting it wrong-lawsuits, patient harm, lost trust-is higher. CMS now requires all Medicare Part D pharmacies to have 99.5% accuracy in Orange Book integration. No exceptions.
The future of drug identification in pharmacy systems
The FDA is rolling out a new machine-readable API for the Orange Book, with real-time updates. That means no more 2-3 week delays between a generic’s approval and its appearance in your system. By 2025, AI-powered tools will predict which patients might react poorly to a switch based on their medication history, genetics, and even past adverse events. The FDA’s Precision Medicine Initiative is already testing whether genetic markers can help decide when a brand is truly necessary.
Meanwhile, the market for pharmacy identification software is growing fast-$1.4 billion in 2023, projected to hit $2.8 billion by 2028. Companies like LexID and Medi-Span are leading the way, with accuracy rates above 99.9%. But the real winners will be the pharmacies that combine smart tech with clear communication and trained staff.
What you can do today
You don’t need a billion-dollar system to get this right. Start here:
- Check your system’s TE code integration. Are you using the latest Orange Book data?
- Set defaults to generics for non-NTI drugs. Make NTI drugs require override.
- Train your team on authorized generics and branded generics. Use the FDA’s list of first approvals.
- Add a patient handout or digital message explaining why generics are safe and equivalent.
- Review your state’s substitution laws monthly. They change.
Generic drugs aren’t second-rate. They’re rigorously tested, widely used, and proven safe. But only if the system-and the people using it-know how to handle them right.

10 Comments
I’ve seen patients panic when their lisinopril switched from blue to white pills. No one explained it. Just handed them a new bottle and said 'it’s the same.'
Simple patient handouts? Game changer.
Oh wow. A 147-adverse-event report? Guess the FDA’s ‘identical’ claim is just marketing fluff wrapped in a lab coat. Who knew generics were just brand-name drugs with a discount tag and a side of chaos?
America spends billions on generics to save money, then lets some tech company in Ohio mess up the NDC codes? This is why our healthcare’s a dumpster fire. We need American-made software, not some third-party API that can’t tell a BX from a AB.
Fix the system or go back to brand-only. No more half-measures.
In India, we don’t have brand vs generic confusion-because generics are the only option. But patients still trust the color and shape. If your system doesn’t reflect that, it’s useless.
I work at a pharmacy and I swear, half the time the system shows ‘authorized generic’ but the label says ‘brand.’ Patients come back crying because they think they got ripped off. And no one in IT cares. I’ve filed 12 tickets. All ignored.
The FDA’s Orange Book? LOL. That’s just a glorified spreadsheet. Did you know Big Pharma pays to get their generics listed as ‘AB’ even when they’re not fully bioequivalent? I’ve seen the emails. It’s all rigged. And now they want AI to fix it? 😂
Wake up, people. This is a profit play, not a safety play.
It is imperative that we prioritize patient education as a foundational element of pharmaceutical care. When individuals are informed of the rigorous standards governing generic medications, their confidence in treatment adherence increases exponentially.
May we all strive to embody compassion and clarity in our professional interactions.
Y’all act like this is some new revelation. Nah. I’ve been screaming this since 2018. The system ain’t broken-it’s designed to confuse. Authorized generics? Branded generics? TE codes? Most pharmacists can’t even spell ‘bioequivalence’ without Google. And don’t get me started on the ‘dye allergy’ blind spot. We’re one FDA audit away from a nationwide meltdown. 🤯
I work in a small clinic in Delhi. We use generics because we have to. But we also print out a 1-pager for every patient: ‘This is the same medicine, just cheaper. No magic, no secret. Just science.’ Works every time. No drama. Just trust.
The fundamental flaw in contemporary pharmacy informatics lies not in technological limitations, but in the epistemological disregard for the phenomenological experience of the patient. One cannot reduce therapeutic equivalence to NDC codes and TE classifications without engaging the hermeneutics of patient perception. The algorithm cannot comprehend fear.