How to Avoid Transcription Errors from E-Prescribing Systems
Every year, thousands of patients in the U.S. face avoidable harm because a prescription got lost in translation-not between languages, but between computer systems. Even though e-prescribing was supposed to eliminate messy handwriting and human mistakes, it created a new kind of error: transcription errors. These happen when a prescription moves from a doctor’s EHR to a pharmacy’s system, and something gets misread, misformatted, or missed entirely. It’s not about typos. It’s about systems that don’t talk to each other properly.
Why E-Prescribing Still Causes Errors
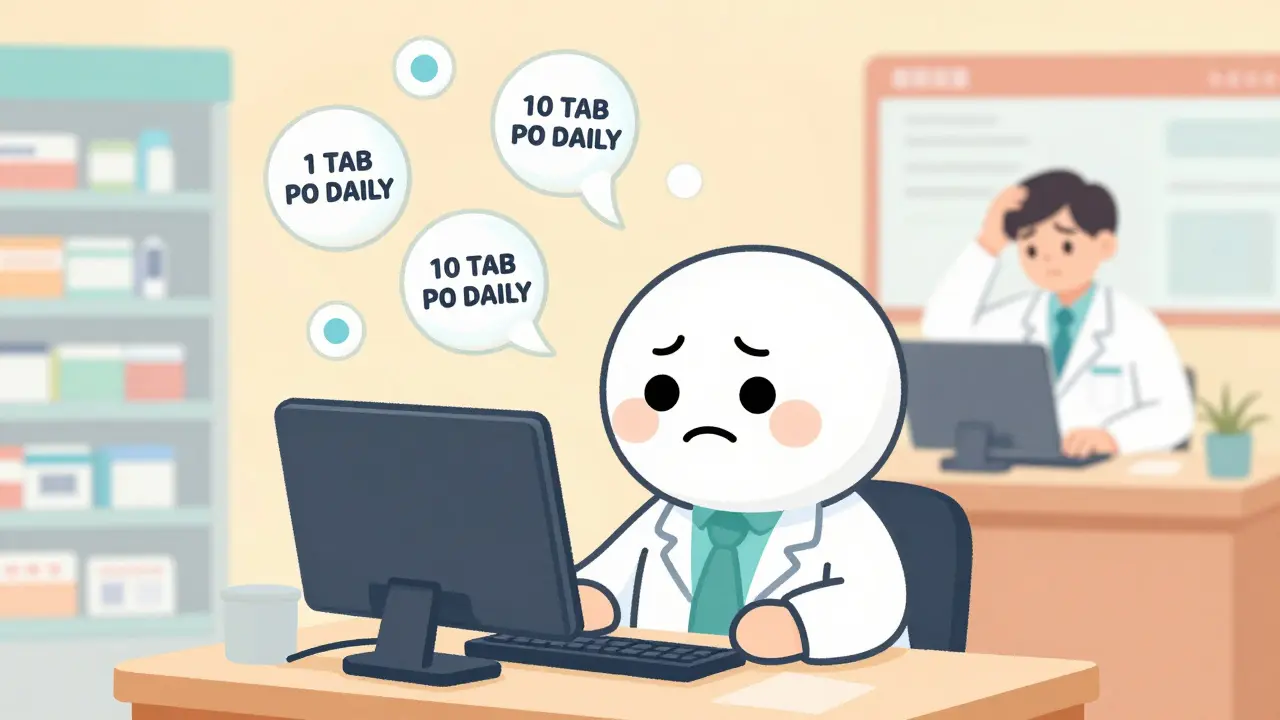
E-prescribing was meant to cut prescribing errors by 80%. And it did-sort of. Studies show it slashed overall errors from 42.5 per 100 prescriptions down to 6.6. But here’s the catch: among the errors that still happen, 37% to 41.5% are transcription errors. That’s not a small number. It means nearly half of all mistakes now come from digital systems miscommunicating. Take this real example: A doctor writes “Take 1 tablet by mouth daily.” The EHR sends it as “1 TAB PO DAILY.” The pharmacy’s system reads “TAB” as “10” because of an old coding quirk. Suddenly, the patient gets 10 pills instead of 1. That’s not a typo. That’s a system failure. The biggest culprits? Fragmented systems. Many clinics use standalone e-prescribing tools like DrFirst Rcopia. Hospitals use Epic or Cerner. Pharmacies use QS/1 or Pioneer. These systems don’t always speak the same language. Even when they’re supposed to, they often don’t. A 2022 Surescripts report found that 41% of pharmacists spend 15 to 30 minutes a day just fixing e-prescription glitches.Standardizing the Prescription Instructions (Sig)
One of the most powerful fixes is standardizing how dosing instructions are written. Instead of letting doctors type free-form text like “take one pill every morning,” systems should force them to pick from preset options: “once daily,” “twice daily,” “every 8 hours,” etc. A 2018 Health Affairs study showed that when clinics used structured sig formatting, transcription errors dropped by 41%. Why? Because systems don’t guess. They read exact codes. “1 TAB PO QD” becomes a machine-readable instruction, not a human interpretation. No more confusing “QD” with “QID.” No more mistaking “PO” for “PR” (oral vs. rectal). It’s simple. It’s precise. And it works. The National Council for Prescription Drug Programs (NCPDP) SCRIPT Standard Version 201900 was built for this. It defines exactly how dosing, route, frequency, and duration should be encoded. Any system claiming to be compliant should follow it. If yours doesn’t, ask why.Use CancelRx to Prevent Confusion
How many times has this happened? A doctor changes a patient’s medication, sends a new e-prescription, but forgets to cancel the old one. The pharmacy gets both. The pharmacist doesn’t know which one to fill. The patient ends up with duplicate meds-or worse, conflicting ones. Enter CancelRx. Developed by Surescripts in 2012, this protocol lets providers electronically cancel a prescription before it’s filled. No more phone calls. No more handwritten notes. No more guessing. Studies show CancelRx cuts discontinued medication errors by 63%. That’s huge. It’s not a fancy AI tool. It’s a simple feature that’s been around for over a decade-and yet, only 58% of practices use it consistently, according to a 2023 KLAS report. If your system doesn’t have CancelRx, it’s outdated.
Link Prescriptions to Medical Indications
Here’s a silent killer: prescribing the right drug for the wrong reason. A patient gets methotrexate for psoriasis. But the system doesn’t say why. So the pharmacist sees “methotrexate 2.5 mg daily” and assumes it’s for rheumatoid arthritis. They refill it every month. But the patient only needs it once a week. That’s a transcription error disguised as a clinical one. Dr. David Bates from Harvard says adding the indication-like “for psoriasis” or “for RA”-could eliminate 78% of dosing frequency errors. It’s not just helpful. It’s life-saving. Systems that support structured indication entry (like Epic’s Hyperspace) reduce indication-drug mismatches by 79%. That’s not a minor improvement. It’s a paradigm shift. If your EHR lets you type “headache” as the reason for a narcotic, but doesn’t force you to pick from a validated list, you’re inviting risk.Get Full Pharmacy-Prescriber Connectivity
The biggest leap forward? Direct, seamless connection between the doctor’s system and the pharmacy’s system. No manual re-entry. No copy-pasting. No screen-switching. A 2017 ISMP Canada case study showed that when systems use HL7 FHIR Release 4.0.1, manual re-entry errors drop by 92%. That’s not theoretical. That’s real. In a pilot with Epic and CVS, transcription errors vanished for 92% of patients because the systems talked directly. But here’s the problem: only 32% of U.S. pharmacies have true interoperability. Most still rely on intermediaries like Surescripts, which help-but don’t fully eliminate-the need for human intervention. If your practice uses a standalone e-prescribing tool, you’re stuck in the old world. Integrated systems like Epic, Cerner, and Allscripts (with direct pharmacy APIs) are where the future is.Fix the Workflow, Not Just the Tech
Technology alone won’t fix this. You need to change how people work. A 2021 AHRQ report laid out six proven strategies:- Standardized sig formatting (cuts errors by 41%)
- CancelRx implementation (cuts discontinued errors by 63%)
- Single shared medication list (cuts reconciliation errors by 52%)
- Structured indication entry (cuts mismatches by 79%)
- Direct pharmacy-prescriber connectivity (cuts re-entry by 92%)
- Redesigned workflow for prescription changes (cuts confusion by 67%)

Watch Out for Alert Fatigue
Doctors get hundreds of alerts a day. “Drug interaction warning.” “Allergy alert.” “Duplicate therapy.” Most are ignored. That’s alert fatigue. And it’s a silent driver of transcription errors. Dr. Joan Ash from Oregon Health & Science University told the FDA that 34% of transcription errors happen because providers override warnings without reading them. They’ve been conditioned to click “OK” and move on. The fix isn’t fewer alerts. It’s smarter alerts. Systems should prioritize based on severity. A warning about a life-threatening interaction should stop the workflow. A warning about a mild interaction should be a quiet note. If your system blasts every possible alert with the same red flag, you’re part of the problem.What You Can Do Right Now
You don’t need to wait for a system upgrade. Here’s what you can do today:- Check if your EHR uses NCPDP SCRIPT 201900. If not, ask your vendor when they’ll support it.
- Make sure CancelRx is enabled and used for every medication change.
- Require indication entry for every prescription. Don’t let “unknown” or “headache” slide.
- Ask your pharmacy: Do they receive prescriptions directly from your system? Or do they have to retype them?
- Train your staff: 4.7 hours of focused training can cut errors by more than half.
- Report errors. If a prescription comes back garbled, document it. Track patterns. Push for fixes.
The Future Is FHIR
The next big shift is HL7 FHIR. It’s not magic. But it’s the closest thing we have to a universal language for health data. The ONC’s 2023 Interoperability Roadmap requires all e-prescribing systems to use FHIR by 2025. Pilots using FHIR for prescriptions (like the Da Vinci Project) have shown 98% error reduction. AI tools are coming too. Epic’s DoseMeRx, now in pilot, uses machine learning to predict dosing errors before they happen. Early results show it can cut transcription errors by another 65% by 2026. But here’s the truth: none of this matters if systems still can’t talk to each other. Until every doctor, hospital, and pharmacy speaks the same digital language, transcription errors will keep happening. The technology exists. The standards are ready. What’s missing is the will to use them fully.What are the most common transcription errors in e-prescribing?
The most common errors include misformatted dosing instructions (e.g., "1 TAB PO DAILY" misread as "10 TAB PO DAILY"), missing medication indications leading to incorrect refills, duplicate prescriptions because CancelRx wasn’t used, and system-specific coding mismatches (like "QD" vs. "QID"). These errors often occur when systems don’t use standardized data formats like NCPDP SCRIPT 201900 or HL7 FHIR.
Do standalone e-prescribing systems have more errors than integrated ones?
Yes. Standalone systems like DrFirst Rcopia have 42% fewer transcription errors than EHR-integrated systems when used in isolation-but integrated systems like Epic reduce overall prescribing errors by 84% because they connect directly to the patient’s full record. The key is whether the system links to a shared medication list and pharmacy network. Integrated systems with direct pharmacy APIs reduce transcription errors by 55% more than standalone tools.
Can e-prescribing systems be hacked to cause transcription errors?
While not common, cyberattacks targeting EHRs or pharmacy systems could alter prescription data during transmission. This is why HIPAA-compliant encryption and audit logs are mandatory. The bigger risk isn’t hacking-it’s poor interoperability. Most errors come from systems misinterpreting each other’s data, not malicious intent. But security gaps can make those errors worse.
Why do pharmacies still manually correct e-prescriptions?
Because 68% of pharmacists say incompatible formatting is the main cause. Even when a prescription is sent electronically, it might use non-standard abbreviations, missing fields, or outdated code sets. Systems that don’t follow NCPDP SCRIPT 201900 or HL7 FHIR force pharmacists to interpret and fix the data manually. This is why 41% of pharmacists spend 15-30 minutes daily on these corrections.
Is there a legal requirement to use error-free e-prescribing systems?
Yes. The 21st Century Cures Act (effective April 2021) bans information blocking-meaning providers and vendors can’t prevent seamless data exchange. The DEA also requires electronic transmission of controlled substances (EPCS). Failure to comply can result in Medicare Part D penalties and loss of certification. While there’s no direct fine for transcription errors, failing to use certified, interoperable systems puts you at risk of regulatory action and liability.
How can small practices afford to fix these errors?
The ONC has allocated $15 million in funding to help small practices (<10 providers) adopt FHIR-based e-prescribing by 2025. Many EHR vendors now include basic interoperability features at no extra cost if you’re on a certified platform. Start with free tools: enable CancelRx, use structured sigs, and connect to Surescripts’ Pharmacy Health Information Exchange, which reduced errors by 88% in pilot programs. You don’t need a $1 million upgrade-just the right settings turned on.

9 Comments
Just saw a pharmacist spend 22 minutes on the phone fixing a prescription because the EHR sent 'QD' instead of 'daily.' We’ve had this solution for years-NCPDP SCRIPT 201900, CancelRx, structured sigs-but nobody’s enforcing it. It’s not a tech problem. It’s a culture problem.
Of course this keeps happening. Doctors don’t care about standards-they care about clicking through their EHR as fast as possible. And vendors? They’d rather sell you a shiny new module than fix the damn interoperability that’s been broken since 2010. Wake up, healthcare. This isn’t ‘innovation.’ It’s negligence dressed up as progress.
My cousin almost got double-dosed because her old script wasn’t canceled. She didn’t even know she had two prescriptions active until the pharmacy called. This isn’t rare. It’s routine. We need to stop treating patient safety like an afterthought.
Let me tell you something funny-my clinic uses DrFirst, and our pharmacy uses QS/1. They ‘talk’ via Surescripts, but only if the moon is in the seventh house and Jupiter aligns with Mars. Last week, ‘Take one tablet twice daily’ became ‘Take 1 TAB BID’ which the system read as ‘Take 10 TAB BID’ because someone in 1998 coded ‘TAB’ as ‘10’ in their legacy system and no one ever fixed it. We’ve all just learned to laugh it off. That’s not resilience. That’s surrender.
I work in a small pharmacy. We get 3-5 of these messed-up e-scripts a day. Sometimes I have to call the doctor’s office three times just to confirm the dose. It’s exhausting. And honestly? I’m tired of being the human error-correction layer for broken software.
While the technical solutions outlined here are robust and evidence-based, it is imperative to recognize that systemic adoption remains hindered by institutional inertia and a lack of standardized enforcement mechanisms. The NCPDP SCRIPT 201900 standard, for instance, is not merely a recommendation-it is a foundational requirement for interoperable health information exchange. Without regulatory alignment and vendor accountability, even the most elegant protocols remain theoretical constructs.
Y’all are overcomplicating this. If your EHR doesn’t have CancelRx turned on by default, switch vendors. If your sigs aren’t picklists, demand it. If your pharmacy still has to call you, you’re doing it wrong. This isn’t rocket science-it’s basic hygiene. 4.7 hours of training? That’s less than a lunch break. Do the work. Patients are counting on you.
Of course you’re all talking about tech fixes. But nobody’s talking about the fact that doctors are overworked, underpaid, and trained to treat the EHR like a checklist, not a tool. You want fewer errors? Hire more staff. Reduce charting burden. Pay providers fairly. Stop pretending software alone can fix a system designed to burn people out. This isn’t a bug. It’s a feature of capitalism.
Exactly. Tech won’t fix human burnout. But good tech can reduce the friction that makes burnout worse. I’ve seen docs use structured sigs and CancelRx and suddenly have 20 extra minutes a day because they’re not chasing down pharmacy calls. That’s not just safety-it’s sanity. Let’s stop pitting tech against compassion. We need both.