How to Read Prescription Labels for Inhalers, Patches, and Injectables
Why Reading Prescription Labels for Inhalers, Patches, and Injectables Matters
It’s not enough to know you’re taking a medicine. With inhalers, patches, and injectables, how you use it can mean the difference between relief and danger. These aren’t pills you swallow with water. They’re precision tools - and if you misread the label, you could be underdosing, overdosing, or even putting yourself at risk of overdose or infection.
In 2022, over 1,400 serious adverse events in the U.S. were linked to people using these devices wrong. A 2023 study found that nearly 4 out of 10 patients misunderstood key parts of their labels. That’s not because they’re careless - it’s because the labels are confusing, inconsistent, or packed with tiny print.
Here’s what you actually need to know to use these medications safely.
Inhaler Labels: What the Numbers Really Mean
Inhalers look simple - a metal canister with a mouthpiece. But the label holds critical details most people miss.
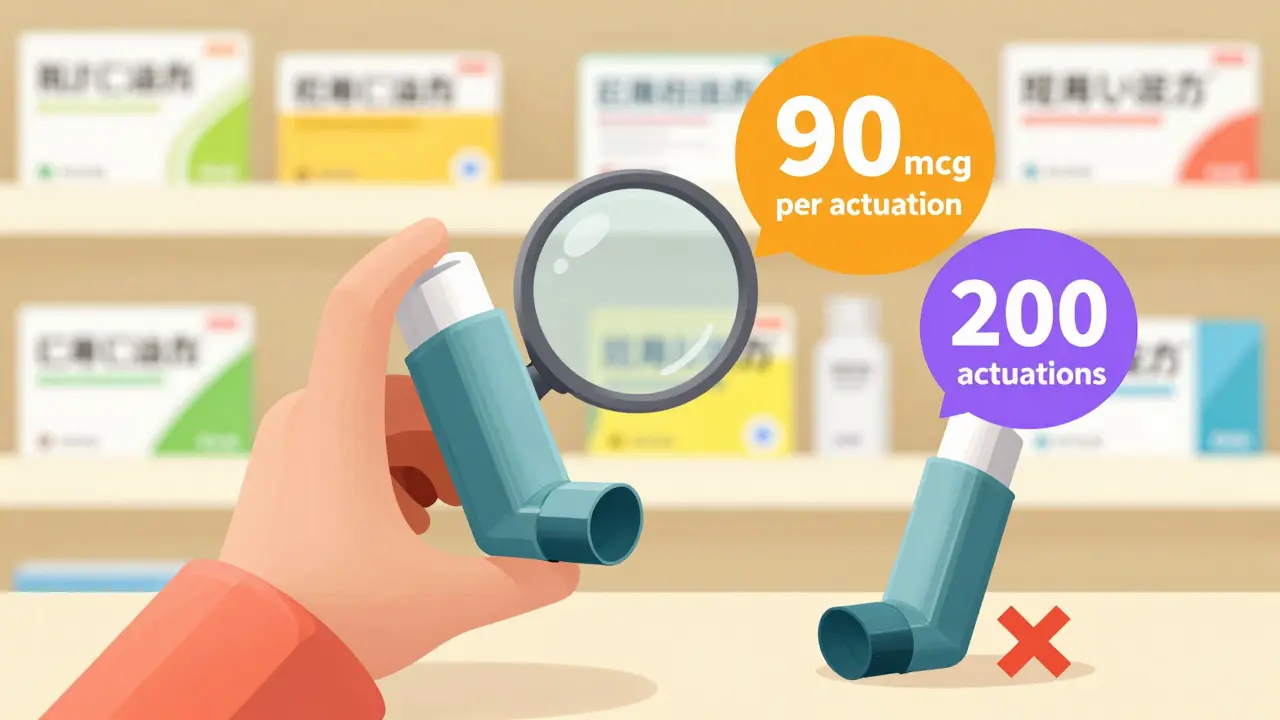
- Dosage per puff: Look for phrases like “albuterol sulfate 90 mcg per actuation.” That’s the amount delivered each time you press down. Never assume it’s the same as your old inhaler.
- Total puffs: The label says “200 actuations.” That doesn’t mean it lasts 200 days. If you use two puffs twice a day, that’s 4 puffs daily - you’re out in 50 days. Many people keep using an inhaler long after it’s empty because the canister still feels heavy. That’s dangerous.
- Prime before first use: New inhalers need 4 test sprays into the air before you use them for the first time. Skipping this means your first few puffs might be air, not medicine.
- Shake well: Only applies to suspension inhalers (like most asthma inhalers). Solution inhalers (like some COPD meds) don’t need shaking. If you shake a solution inhaler, you’re wasting time and possibly making it harder to inhale properly.
- Dose counter: Since May 2024, all new inhalers must have a visible counter. If yours doesn’t, ask your pharmacist for a replacement. Older inhalers without counters are still in use - and they’re the most common source of accidental underdosing.
Pro tip: If your inhaler looks the same as someone else’s - even if the name is different - don’t swap them. Labels may look identical, but the dosage can vary wildly.
Patch Labels: More Than Just Stick and Forget
Transdermal patches seem easy: peel, stick, wait. But the label holds hidden rules.
- Delivery rate: Fentanyl patches say “25 mcg/hour.” That’s the amount released every hour, not the total dose. A 72-hour patch releases 1,800 mcg total. That’s a lot. Never cut a patch - cutting it can release up to 4.7 times more medication at once, leading to overdose.
- Wear time: “Change every 72 hours” means exactly 72 hours. Not “about three days.” If you change it at bedtime on Monday, change it at bedtime on Thursday. Drifting by a few hours can cause dangerous spikes or drops in medication levels.
- Application site: Always apply to clean, dry, hairless skin. Avoid areas with scars, burns, or irritation. Rotating sites prevents skin reactions. Labels will tell you where - chest, back, upper arm - and where not to put it (like near heat sources).
- Heat warning: Since 2021, all patch labels must warn about heat. Sitting in a hot tub, using a heating pad, or even lying in direct sunlight can increase absorption by up to 50%. That’s enough to cause an overdose, even if you’re taking the right dose.
- Disposal: Fold the patch in half with the sticky sides together and flush it down the toilet. Don’t throw it in the trash. In 2022, the FDA reported 147 cases of accidental exposure - including children and pets - from improperly thrown-out patches.
Many patients don’t realize patches can still leak medicine after removal. Always wash your hands after handling one, even if you think it’s “used up.”
Injectables: Concentration Is Everything
Injectables are the most dangerous if misread. One wrong decimal point can kill.
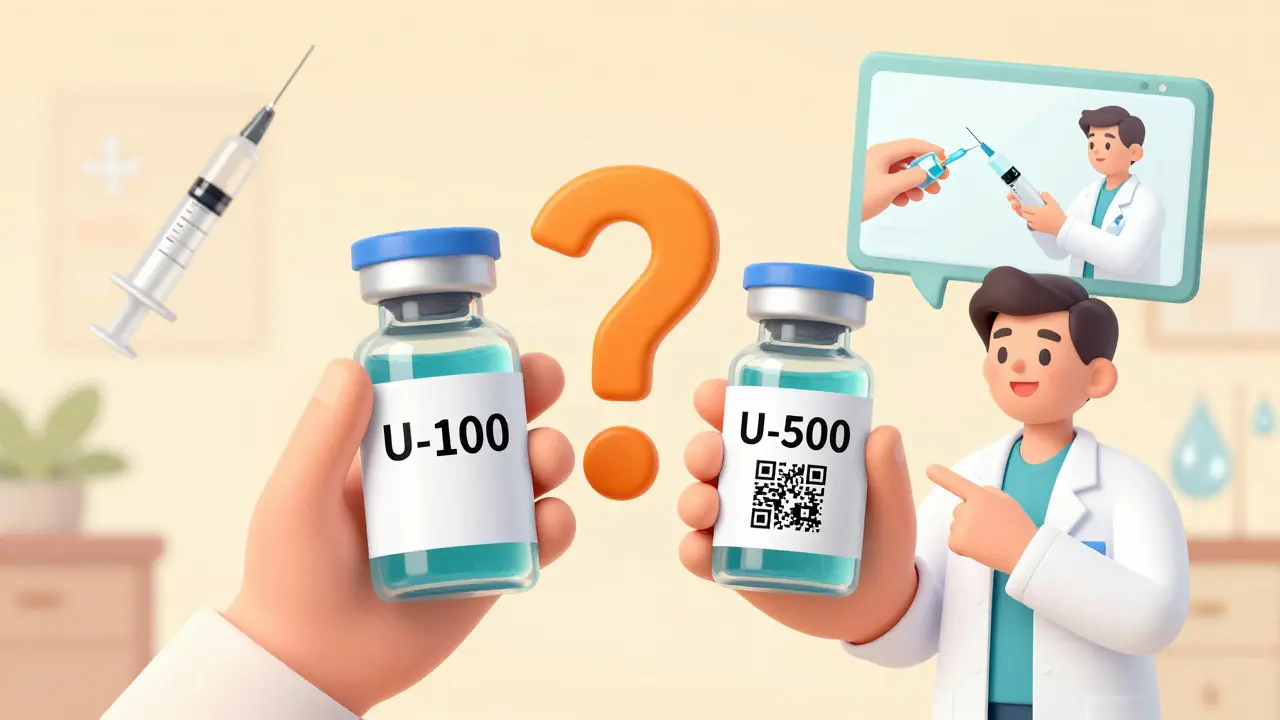
- Concentration: Insulin labels say “U-100.” That means 100 units per milliliter. But some insulin is U-500 - five times stronger. If you think you’re taking 10 units of U-100 but grab U-500 by mistake, you’ve injected 50 units. That’s a medical emergency.
- Volume vs. total dose: A label might say “100 units/mL” and “1 mL per dose.” That’s 100 units total. But if you see “50 units/mL” and “2 mL per dose,” you’re still getting 100 units. Never assume the volume is the dose.
- Reconstitution: Some injectables come as powder and need mixing with liquid. Labels will say “add 1.2 mL of diluent” - not “add water.” Use only what’s provided. Mixing with the wrong fluid can destroy the medication.
- Storage: Some injectables need refrigeration. Others must be kept at room temperature after opening. Check the label. Leaving insulin in a hot car for an hour can ruin it - and you won’t know until you get low blood sugar.
- Needle safety: Labels often include “single-use only.” Reusing needles increases infection risk and changes how the drug delivers. Always dispose of needles in a sharps container - never in the regular trash.
Patients with visual impairments struggle most here. Many vials look identical. Always double-check the name and concentration before drawing up a dose. If you’re unsure, ask your pharmacist to mark the vial with a colored sticker.
What to Look for on Every Label - Even If You Think You Know It
There are five universal red flags on any prescription label for these delivery systems:
- “Do not cut” or “Do not crush”: Especially on patches and some injectables. Cutting changes how the drug releases.
- “For external use only”: If it’s a patch or topical spray, don’t swallow it. Sounds obvious - but people have accidentally ingested fentanyl patches.
- Auxiliary labels: Those small stickers next to the main label say things like “May cause drowsiness” or “Avoid alcohol.” They’re not optional. They’re warnings.
- Visual pictograms: Since 2020, over 78% of inhaler labels now include icons showing how to inhale, hold your breath, or rinse your mouth. Don’t ignore them. A 2023 study found these pictograms cut technique errors by 37%.
- QR codes: More than two-thirds of new prescriptions now have QR codes that link to short videos showing how to use the device. Scan it with your phone. It’s faster than reading.
What to Do If You’re Still Confused
You’re not alone. A 2023 JAMA study found only 38% of patients got a full explanation from their pharmacist. Don’t wait until you’re at home with a half-empty inhaler to ask questions.
- Ask your pharmacist to demonstrate: Say, “Can you show me how to use this?” Most pharmacies have demo devices. Watch closely.
- Take a photo of the label: If you’re worried about forgetting, snap a picture of the label with your phone. Keep it in your medication app.
- Use the “teach-back” method: After your pharmacist explains, say, “So if I use this inhaler, I shake it, press once, breathe in slow, hold for 10 seconds, then rinse?” If they nod, you got it right. If they correct you - listen.
- Check the manufacturer’s website: Search the drug name + “patient instructions.” Most companies have downloadable PDFs with step-by-step videos.
If you’re caring for someone else - a parent, partner, or child - don’t assume they understand. Sit with them and go through the label together. Misuse doesn’t just hurt the user - it burdens the whole system.
The Bigger Picture: Why This Isn’t Just Your Problem
The global market for inhalers, patches, and injectables hit $1.27 trillion in 2023. That’s because these delivery systems are now the go-to for chronic conditions: asthma, diabetes, chronic pain, hormone therapy, and more.
Regulators are trying to fix labeling chaos. The FDA now requires standardized pictograms on all new devices. QR codes are rising fast. By 2027, some labels will use augmented reality - point your phone at the vial, and a 3D video shows you how to inject it.
But until then, you’re the last line of defense. You’re the one holding the device. You’re the one reading the tiny print. You’re the one who has to spot the difference between U-100 and U-500. Don’t let confusion become a mistake.
Final Checklist Before You Use Any of These
- ✔️ Is the medication name and dosage clear?
- ✔️ Do I know how many puffs, hours, or mL to use?
- ✔️ Am I using the right device? (No swapping between similar-looking ones)
- ✔️ Have I checked for heat warnings, disposal rules, or “do not cut”?
- ✔️ Did I scan the QR code or watch the video?
- ✔️ Did I ask a pharmacist to show me how to use it?
If you answer yes to all six, you’re doing better than most. Keep going. Your safety depends on it.
What should I do if my inhaler doesn’t have a dose counter?
If your inhaler lacks a dose counter, ask your pharmacist for a replacement. Older inhalers without counters are still common, but they’re a major cause of accidental underdosing. In the meantime, track your puffs manually - write down each time you use it. Most inhalers have 200 puffs total. Divide that by how many you use per day to estimate how long it will last.
Can I cut my fentanyl patch to lower the dose?
Never cut a fentanyl patch. Cutting it can cause the medication to release too quickly - up to 4.7 times faster - which can lead to overdose, respiratory failure, or death. Even if the patch looks like it’s not working, don’t cut it. Talk to your doctor about switching to a lower-strength patch instead.
Why does my insulin label say U-100? What does that mean?
U-100 means 100 units of insulin per milliliter. This is the standard concentration. But some insulin is U-500 - five times stronger. If you mistake U-500 for U-100 and inject the same volume, you’ll get five times the dose. Always double-check the concentration before drawing up your dose. If you’re unsure, ask your pharmacist to mark the vial with a colored sticker.
How do I know when my patch is done if it still sticks?
Patches don’t always look empty. Even if it still sticks, it may have delivered all its medicine. Always follow the label’s wear time - like “change every 72 hours.” Don’t rely on how it feels or looks. If you’re unsure, check the original prescription instructions or call your pharmacist. Leaving a patch on too long won’t help - it won’t release more medicine once it’s used up.
Is it safe to reuse needles for injectables?
No. Reusing needles increases your risk of infection, skin damage, and inaccurate dosing. The needle dulls after one use, making injections more painful and less precise. It can also cause medication to stick inside the needle, changing how much you actually get. Always use a new needle each time and dispose of it in a sharps container - never in the trash.
What should I do if I accidentally use the wrong inhaler?
If you accidentally use someone else’s inhaler - or the wrong one - stop using it immediately. Call your pharmacist or doctor. Even if you feel fine, the dose might be wrong for your condition. For example, using a high-dose steroid inhaler instead of a rescue inhaler can suppress your immune system. Never share inhalers. Always store them in labeled containers.

9 Comments
This is all just a distraction. The real issue is Big Pharma designing these labels to confuse people so they keep buying new ones. They don't want you to understand. They want you dependent.
I read this and immediately thought about my mom’s fentanyl patch. She still cuts it in half because she says it "feels too strong." 😩
The structural inefficiencies inherent in pharmaceutical labeling protocols are not merely inconveniences-they are systemic failures of risk communication. The absence of standardized tactile indicators for visually impaired patients constitutes a profound violation of accessibility ethics. Moreover, the reliance on QR codes as a primary pedagogical tool assumes universal digital literacy-a privilege not universally held.
You people are lucky if you even have access to a pharmacist who explains anything. My last prescription came with a label written in Latin and a QR code that linked to a 12-minute ad for the drug manufacturer. This isn’t healthcare. It’s a trap.
i realy didnt know about the heat thing with patches... i put mine on my arm and sit by the window a lot... hope i didnt mess up...
The fact that you're still using "actuation" instead of "dose delivery event," and that you're not citing the ISO 11608-1:2023 standard for inhaler labeling, suggests a fundamental lack of rigor. Also, why no mention of the EU’s EudraLex Annex 11 compliance? This article reads like a pamphlet from a pharmacy intern.
thanks for the heads up on the qr codes. i scanned mine last night and it showed a video of how to use my inhaler. i had no idea i was breathing wrong. kinda embarrassing but also kinda helpful.
It is imperative that patients understand that the misuse of injectables, particularly insulin, constitutes a gross negligence of personal responsibility. The fact that so many individuals rely on color-coded stickers rather than medical training is not only alarming-it is indefensible. You are not a scientist. You are a patient. Trust the professionals.
This is the kind of info that changes lives. I used to be scared to use my insulin pen because I didn’t understand the numbers. Now I know U-100 isn’t magic-it’s just a ratio. If you’re reading this and still unsure, reach out. Someone’s got your back.