How to Talk to Doctors About Senior Medications: A Clear Guide for Patients and Caregivers

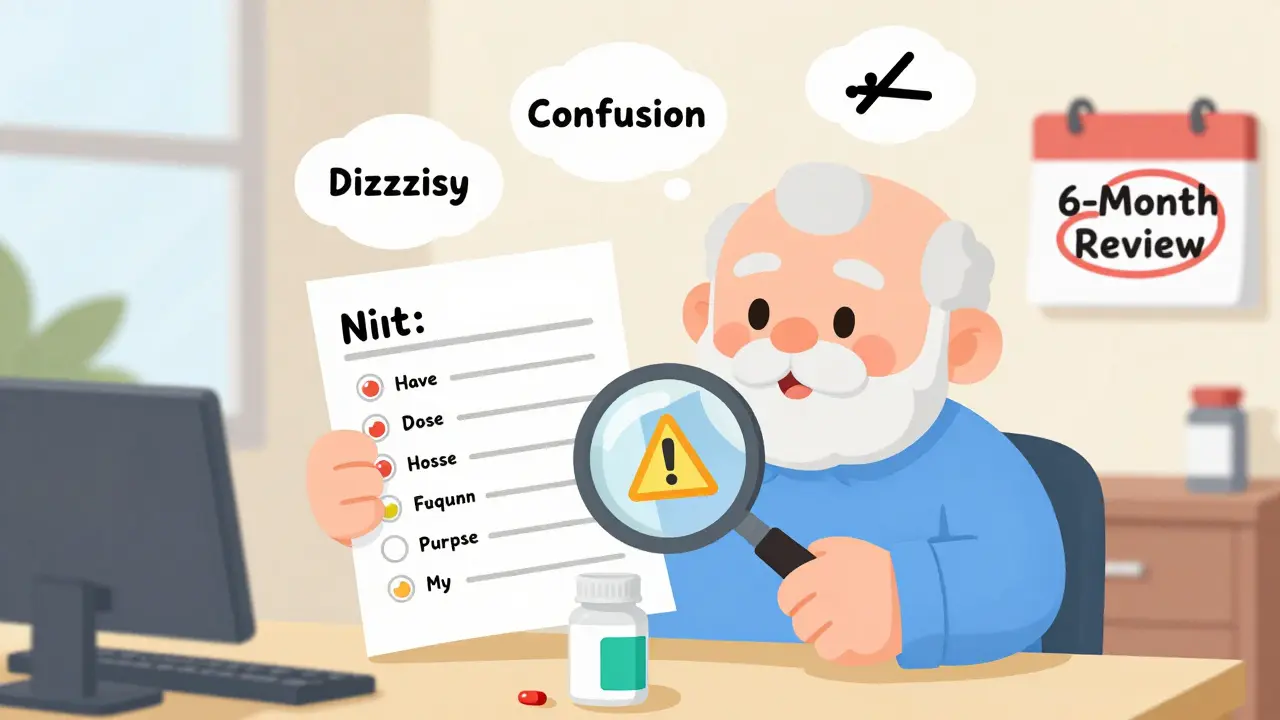
When you or a loved one is taking five or more medications, it’s easy to feel overwhelmed. You might forget why you’re taking one pill, worry about side effects, or wonder if something’s missing. The truth is, senior medications aren’t just about prescriptions-they’re about safety, clarity, and control. And the most powerful tool you have isn’t a pill organizer or app-it’s your conversation with your doctor.
Why Medication Talks Matter More Than Ever
About 89% of adults over 65 take at least two prescription drugs. One in seven takes five or more. That’s not unusual-it’s normal. But with every added medication, the risk of harmful interactions, side effects, and hospital visits goes up. In fact, medication problems send over 350,000 seniors to the hospital every year in the U.S. Most of these aren’t accidents. They’re the result of miscommunication. The good news? Simple, structured conversations with your healthcare provider can cut those hospitalizations by nearly a quarter. You don’t need to be an expert. You just need to show up prepared.Before the Appointment: Get Your Medication List Ready
Don’t rely on memory. Don’t say, “I think I take something for blood pressure.” Bring the actual bottles. Or better yet, bring everything you take in a single bag: prescription pills, over-the-counter pain relievers, vitamins, herbal supplements, even eye drops or creams. Why? Because studies show that when patients bring their real medications to appointments, doctors find discrepancies-wrong doses, discontinued drugs still listed, duplicates-in 25% of cases. That’s one in four seniors. Make a written list with:- Drug name (use the label from the bottle)
- Dose (e.g., 10 mg, not “one pill”)
- How often (e.g., “once daily at breakfast”)
- Purpose (e.g., “for high blood pressure,” “for arthritis pain”)
Bring Someone With You
It’s not weak to bring a family member, friend, or caregiver. It’s smart. During appointments, stress, noise, or medication side effects can make it hard to focus. Someone else can listen, take notes, and ask questions you might forget. Research shows seniors who bring a companion have 18% fewer adverse drug events. That’s not a small number. That’s life-changing.Ask These Four Questions Every Time
You don’t need to sound like a doctor. Just ask these four things:- “How does this medication specifically help manage my health condition?”-You deserve to know why you’re taking it, not just that you’re supposed to.
- “What are the potential side effects and adverse reactions?”-Not just the common ones. Ask about dizziness, confusion, falls, or changes in appetite. These are often dismissed as “just aging,” but they might be drug-related.
- “What are the drug interactions and potential conflicts?”-Especially if you’re seeing multiple doctors. A new painkiller from your orthopedist might react badly with your heart medication from your cardiologist.
- “What should I do if I miss a dose?”-Some pills are okay to skip. Others can be dangerous. Don’t guess.
Use the Teach-Back Method
After your doctor explains something, say: “Just to make sure I got it right-so if I take this pill at night, I shouldn’t drink grapefruit juice, and if I feel dizzy, I should call you?” This is called the teach-back method. It’s not about testing you. It’s about making sure the doctor knows you understood. Studies show this technique improves adherence by 31%. That means you’re more likely to take your meds correctly-and less likely to end up back in the hospital.Review Everything Every Six Months
Medications aren’t set in stone. Your body changes. Your conditions change. What worked a year ago might not be right now. Ask your doctor: “Is everything I’m taking still necessary?” Many seniors are on drugs they don’t need anymore. Maybe their blood pressure improved. Maybe their joint pain got better with physical therapy. Maybe the original reason for the pill doesn’t exist anymore. But the prescription keeps rolling. A 2022 study found that regular medication reviews reduce polypharmacy (taking too many drugs) by 27%. That’s a huge win for safety and quality of life.Use Tools to Stay on Track
You can’t remember everything. That’s why tools exist.- Pill organizers-Simple ones with morning, afternoon, evening, and night slots work wonders.
- Medication apps-Apps like Medisafe or Round Health send reminders and let you track side effects. Some even alert your pharmacist if you miss a dose.
- Automated dispensers-Devices that open at set times and lock until it’s safe to take the pill. Great for memory issues.
- Medication synchronization-Ask your pharmacy if they offer this. It means all your refills are due on the same day each month. No more juggling 10 different pickup dates.
Speak Up About Side Effects
Dizziness? Confusion? Dry mouth? Constipation? Fatigue? These aren’t “just getting older.” They’re signals. One senior I know started taking a new blood pressure pill and began falling every few days. She didn’t mention it because she thought it was normal. Three months later, she broke her hip. Turns out the medication lowered her blood pressure too much when she stood up. Tell your doctor about every change-even if it seems small. Write it down between visits. Keep a notebook by your bed. Note when you feel off, what you took, and what time.
Know the Beers Criteria
The American Geriatrics Society updates a list called the Beers Criteria every few years. It’s a guide to medications that are risky for seniors. The 2023 version lists 30 drug classes to avoid or use with extreme caution-like certain antihistamines, sleep aids, and painkillers. You don’t need to memorize the list. But if your doctor prescribes something you’ve never heard of, ask: “Is this on the Beers Criteria?” They might say yes-and explain why it’s still right for you. Or they might realize they forgot to check and switch to something safer.What If Your Doctor Dismisses Your Concerns?
Sometimes, doctors rush. Sometimes, they assume you’re “just old.” Don’t accept that. Say: “I’ve read that this drug can cause confusion in older adults. Can we talk about alternatives?” If they brush you off, ask for a referral to a geriatrician or a pharmacist who specializes in senior medications. Many hospitals have medication therapy management programs-free for Medicare patients. They’ll review your entire list, spot problems, and call your doctor with suggestions. You’re not being difficult. You’re being responsible.It’s Not Just About Pills-It’s About Living Well
Taking fewer medications doesn’t mean giving up care. It means getting the right care. It means fewer side effects. Fewer falls. More energy. More time with family. One woman in Austin, 78, was taking 11 medications. After a medication review, her doctor removed three that weren’t helping, adjusted two doses, and switched one for a safer alternative. Within six weeks, she stopped feeling dizzy. She started walking again. She said, “I didn’t realize I’d been living with foggy thinking for two years.” Your medications should help you live-not limit you.What should I do if I don’t understand what my doctor says about my medications?
Ask them to explain it again using simpler words. Say, “Can you explain that like I’m not a doctor?” Write down what they say. If you’re still unsure, ask for written instructions or a printed handout. You can also ask to speak with the pharmacist-they’re trained to explain medications clearly. Many pharmacies offer free consultations.
Can I stop a medication if I think it’s causing problems?
Never stop a prescription on your own. Some drugs need to be tapered off slowly to avoid serious withdrawal effects. Instead, write down your concerns-when the side effect started, how often it happens, and how it affects your daily life. Bring that list to your next appointment and ask: “Can we try reducing this or switching to something else?”
How often should I review my medications with my doctor?
At least once every six months, or whenever you start or stop a medication. If you’ve recently been hospitalized or had a major change in health (like a fall or new diagnosis), schedule a review right away. Medicare now requires a full medication review for patients taking eight or more drugs.
Are over-the-counter drugs and supplements really a big deal?
Yes. Many seniors take OTC painkillers like ibuprofen daily, not realizing they can raise blood pressure or damage kidneys. Supplements like St. John’s Wort can cancel out antidepressants or blood thinners. Even calcium supplements can interfere with thyroid meds. Always list everything-even “natural” products.
What if I can’t afford all my medications?
Tell your doctor. They can often switch you to a generic version, prescribe a lower dose that can be split, or connect you with patient assistance programs. Some pharmacies offer $4 generic lists. Medicare Part D also has a low-income subsidy program. Never skip doses because of cost-there are solutions, but only if you speak up.
Next Steps: Start Today
You don’t need to fix everything at once. Start with one thing:- Today, gather all your medications in one bag.
- Tomorrow, make a simple list with names, doses, and why you take them.
- Next week, bring that list to your next appointment and ask: “Is everything I’m taking still necessary?”

14 Comments
This article hit me right in the chest. My mom was on 12 meds until we brought her bottles to the appointment and found three she hadn't taken in over a year. One was for a thyroid issue she’d recovered from five years prior. The doctor just kept prescribing it. She stopped those three and started sleeping through the night for the first time in years. No more daytime fog. No more falling. Just her again.
Of course you need to bring your meds. But let’s be real-most doctors don’t have time to go through a bag of pills. They glance at the list, nod, and write another script. This whole thing is performative. The system is broken. You’re just supposed to survive it.
Y’all ever notice how every doc says ‘take it with food’ but never says what food? Like, is a cracker enough? Do I need a full sandwich? I once took my blood pressure med with a bag of chips and felt like a ghost for three hours. Also, why do they call it ‘polypharmacy’ like it’s a fancy word? It’s just too many pills. Plain and simple.
And don’t get me started on the ‘natural’ supplements. My aunt took turmeric for her knees and ended up in ER because it messed with her blood thinner. She thought it was ‘just spice.’
My dad’s pharmacist in Montreal did a full med review for free. No appointment needed. Just walked in with his bottles. She spent 45 minutes with him, flagged three interactions, and called his doctor on the spot. Why can’t we do this here? Why is it a privilege to have someone actually look at your meds?
Canada’s not perfect, but we don’t make seniors jump through hoops to stay alive.
STOP. STOP. STOP. You think this is about pills? It’s about CONTROL. The pharmaceutical companies know you’re scared. They know you’re lonely. They know you’ll take anything that promises to fix you. That’s why they push so many drugs. They profit from your fear. And your doctors? They’re paid by the script. Not by your health.
That Beers Criteria? It’s not a guide-it’s a warning label on a system that’s been rigged for decades. You think your doctor’s helping you? They’re just following the script. Literally.
My neighbor’s daughter said she’s got a secret app that tracks if your meds are fake. I don’t know if it’s true but she says the FDA lets bad pills in and no one checks. She says if you take too many pills, your body starts rejecting them and you get sick for no reason. I’m scared now. Should I stop all my meds?
They don’t want you to know this-but there’s a hidden database. Every time a senior is hospitalized for a med reaction, it gets buried under ‘age-related complications.’ The CDC knows. The AMA knows. But they won’t say it out loud. Why? Because if people realized how many of these deaths are preventable, the whole system would collapse. Pills are big business. And we’re the product.
I’ve seen it. My uncle died after a ‘routine’ med change. The death certificate said ‘natural causes.’ He was 74. He took 9 pills. Three of them were new. That’s not natural. That’s negligence.
Medication isn’t medicine. It’s a distraction from the real problem: we’ve abandoned our elderly. We’ve outsourced care to pills because we don’t have the time, the empathy, or the infrastructure to actually care for people. We treat symptoms like puzzles to solve, not humans to hold. This guide? It’s a Band-Aid on a severed artery.
You can ask the four questions all you want. But if your doctor’s on a 10-minute timer, if they’re burned out, if they’re paid by volume-not by outcomes-then your ‘rights’ are just words on a screen. The system doesn’t care if you live. It cares if you’re billed.
I’ve been helping my grandma with her meds for years. The biggest thing I learned? It’s not about remembering the pills. It’s about remembering the person behind them. She used to tell me stories about her garden while we sorted her pills. Now she just stares at the bottle. That’s the real cost of polypharmacy-not the side effects. It’s the silence.
When we cut down her meds, she started humming again. Not because she felt better physically. But because she felt seen. That’s what this guide misses. The humanity.
OMG YES. I brought my 82-year-old mom to her appointment with a Tupperware full of bottles and she cried because the doctor actually looked at them. 😭 I’m telling everyone. This is the most important thing I’ve ever shared. #MedicationRevolution 🙏💊
One correction: the Beers Criteria doesn’t list 30 drug classes-it lists 34 in the 2023 update. Also, ‘Round Health’ isn’t a real app. You might mean ‘Round’ or ‘Medisafe.’ Accuracy matters when lives are at stake. And yes, pharmacists are underutilized. They’re the most accessible medication experts in the healthcare system.
Bring your meds. Ask questions. Review every six months. These are good points. But the real issue is the lack of primary care access. If seniors had regular appointments with their own doctor instead of rotating specialists, most of these problems would resolve themselves. The system is fragmented. The advice is sound. The structure is broken.
I love how this guide assumes everyone has someone to bring with them. What if you’re alone? What if you’re widowed, have no family, and can’t afford a ride? The advice is great. But it’s written for people who have privilege. The real heroes are the home care workers who show up at 7am with a pill organizer and a hug. They’re the ones holding this system together.
I’m a retired paramedic. I’ve seen too many seniors brought in after a med mix-up. The one thing I always tell families? Don’t wait for the appointment. Call the pharmacy. Ask for a med review. They’re legally required to do it for free under Medicare. No doctor needed. Just call. It takes 15 minutes. It could save your life.