IgA Deficiency: Immune Disorder and Transfusion Precautions

Most people have never heard of IgA deficiency, but it’s one of the most common immune disorders in the world. About 1 in 600 people in Caucasian populations have it. And here’s the twist: most of them don’t even know it. You could live your whole life with selective IgA deficiency and never have a single symptom. But if you need a blood transfusion? That’s when things get dangerous.
What Exactly Is IgA Deficiency?
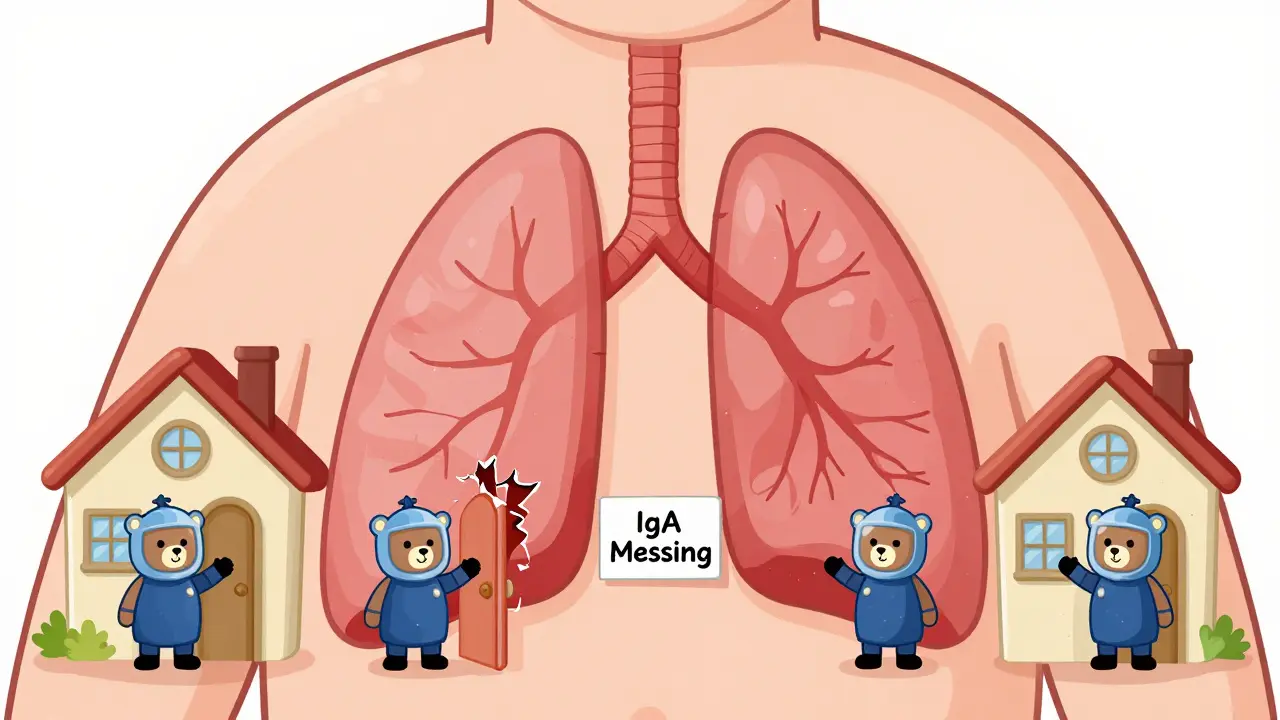
Immunoglobulin A, or IgA, is the body’s first line of defense in your mouth, nose, lungs, and gut. It’s the antibody that keeps germs from sneaking in through your mucous membranes. Normally, IgA makes up about 15% of all your antibodies. In IgA deficiency, your body either produces almost none of it-or none at all. The official cutoff? Serum levels below 7 mg/dL. Everything else-like IgG and IgM-stays normal. That’s what makes it "selective." Your immune system isn’t broken overall. It’s just missing one key piece.It’s usually inherited. If someone in your family has it, your risk jumps by about 50 times. But it’s not always passed down. Sometimes it just happens. And unlike secondary IgA deficiency (caused by drugs like phenytoin or sulfasalazine), this one sticks with you for life.
Most People Don’t Know They Have It
Here’s the surprising part: 90 to 95% of people with IgA deficiency never have problems. No infections. No allergies. No autoimmune issues. They get sick like anyone else-cold, flu, maybe a stomach bug-but nothing unusual. That’s why so many cases go undiagnosed.But for the 5 to 10% who do have symptoms? It’s not mild. Recurrent infections are common. About 1 in 3 people with symptoms get ear infections. Nearly 1 in 4 develop chronic sinusitis or bronchitis. Pneumonia happens too. Then there’s the gut: 1 in 7 deal with chronic diarrhea. Some get giardiasis-a parasitic infection that won’t go away. And about 1 in 10 end up with celiac disease, even if they never had digestive symptoms before.
Allergies are also more common. About 1 in 4 symptomatic patients have eczema, asthma, hay fever, or allergic conjunctivitis. It’s like the immune system, missing its IgA guard, starts overreacting to harmless things.
The Real Danger: Blood Transfusions
This is where IgA deficiency becomes life-threatening. About 20 to 40% of people with this condition develop anti-IgA antibodies. These antibodies don’t cause problems on their own. But if they ever meet IgA in a blood transfusion? Boom.Standard blood products contain IgA. When your body sees it after making antibodies against it, your immune system goes into full attack mode. Reactions happen fast-within minutes. Eighty-five percent of severe reactions occur in the first 15 minutes of a transfusion.
Symptoms? They range from hives and itching to full-blown anaphylaxis. Think: dropping blood pressure, wheezing, swelling, and cardiac arrest. About 15% of these reactions are life-threatening. And in 10% of those cases, they’re fatal.
One study found that transfusion reactions in IgA-deficient patients happen once in every 1,000 transfusions. That might sound rare. But when it happens? It’s catastrophic.
How Do Doctors Know Who’s at Risk?
If you’ve been diagnosed with IgA deficiency, you should be tested for anti-IgA antibodies before any transfusion. The test? An enzyme-linked immunosorbent assay (ELISA). It’s 95% accurate. But here’s the catch: 5 to 10% of the time, it gives a false negative. That means even if the test says "no antibodies," you could still be at risk.That’s why experts recommend a two-step approach: always assume risk if you have IgA deficiency, even if your antibody test is negative. The safest move? Don’t use regular blood.
What Blood Products Are Safe?
There are two approved options:- IgA-depleted blood products: These have less than 0.02 mg/mL of IgA. They’re made by removing IgA from donated blood.
- Washed red blood cells: The plasma and white blood cells are washed away, removing 98% of IgA. This takes extra time-30 to 45 minutes per unit.
Both are expensive. Specialized products can cost up to 300% more than regular blood. And they’re not always available. Ordering IgA-depleted blood can take 48 to 72 hours. In an emergency? That’s not fast enough.
Some hospitals use pre-transfusion medications-like methylprednisolone and diphenhydramine-to reduce reaction risk. These cut reaction rates by 75%. But they’re not foolproof. They’re a backup, not a solution.

What Should You Do If You Have IgA Deficiency?
If you’ve been diagnosed, here’s what you need to do right now:- Get tested for anti-IgA antibodies-even if you’ve never had a transfusion.
- Wear a medical alert bracelet or necklace. It should say: "Selective IgA Deficiency - Requires IgA-Depleted or Washed Blood Products."
- Carry a printed card in your wallet with your diagnosis, transfusion requirements, and your doctor’s contact info.
- Tell every doctor, nurse, and ER staff you meet. Don’t assume they know what IgA deficiency is. A 2023 survey found that 42% of patients had been treated by providers who didn’t know the necessary precautions.
- Get regular screenings for celiac disease, lung damage (like bronchiectasis), and autoimmune disorders. Annual blood tests for tissue transglutaminase antibodies are standard.
Emergency rooms are the most dangerous place for someone with IgA deficiency. Nearly 80% of severe transfusion reactions happen when medical history isn’t available. That’s why your alert ID isn’t optional. It’s your lifeline.
What About New Treatments?
There’s promising research. A new experimental therapy uses recombinant human IgA-lab-made IgA designed to replace what the body can’t make. As of October 2023, only 12 people worldwide had received it. It’s not available yet. But early results show it might prevent infections and reduce the need for transfusions in the future.For now, the best treatment is awareness, preparation, and communication.
Long-Term Outlook
The good news? Most people with IgA deficiency live normal, healthy lives. A 20-year study found that 95% have a normal life expectancy. The 5% who develop serious complications-like severe lung damage or autoimmune disease-may face a 15 to 20% shorter lifespan. But with proper monitoring and care, even those risks can be managed.The key isn’t a cure. It’s knowing your risk. And making sure everyone around you knows it too.
Can IgA deficiency be cured?
No, IgA deficiency cannot be cured. It’s a lifelong genetic condition. But most people don’t need treatment because they have no symptoms. For those who do, management focuses on preventing infections, screening for related conditions like celiac disease, and using special blood products during transfusions to avoid life-threatening reactions.
Is IgA deficiency the same as having no immune system?
No. IgA deficiency is not the same as having no immune system. People with this condition still produce normal levels of IgG and IgM, which handle most systemic infections. The problem is only with IgA, which protects mucosal surfaces. Most people with IgA deficiency fight off colds, flu, and other infections just fine. The real danger comes from transfusions, not everyday illness.
Can I donate blood if I have IgA deficiency?
Yes, you can donate blood. Blood donation centers do not screen donors for IgA deficiency. Since your IgA levels are low, your blood won’t contain enough to cause harm to most recipients. However, if you have anti-IgA antibodies, your plasma could potentially trigger a reaction in someone with IgA deficiency. For this reason, some centers may defer your plasma donations, but whole blood donations are generally accepted.
Do I need to avoid all medications if I have IgA deficiency?
No, you don’t need to avoid medications unless they’re known to cause secondary IgA deficiency (like phenytoin or sulfasalazine). Most drugs are safe. The only real concern is blood products. Always tell your doctor about your IgA deficiency before any procedure involving transfusions, IVIG, or plasma-containing treatments.
Why don’t all hospitals test for anti-IgA antibodies before transfusions?
Testing isn’t universally required because it’s expensive, takes time, and can give false negatives. Some guidelines, like those from the American Association of Blood Banks, recommend testing all IgA-deficient patients. Others, like the European Society for Immunodeficiencies, suggest testing only those with prior reactions. This leads to inconsistent care. That’s why carrying your own medical alert ID is critical-it ensures you get the right treatment no matter where you are.

8 Comments
Okay but let’s be real - this is wild. 1 in 600 people have this and don’t even know it? That’s like finding out half your coworkers are secretly vampires and the only thing that kills them is a blood bag from CVS.
I got chills reading about the transfusion thing. Imagine showing up to the ER after a car crash, and the nurse just plops in regular blood like it’s soda. Boom. Anaphylaxis. No warning. No second chance.
And the fact that 42% of providers don’t even know what IgA is? That’s not negligence. That’s systemic failure. We need a national alert system for this. Like, a badge on your DMV record. "IgA Deficient - DO NOT GIVE PLASMA."
Also, recombinant IgA? That’s sci-fi stuff. We’re basically one step away from lab-grown antibodies in a vial labeled "DO NOT OPEN." I’m here for it.
This is the most terrifying thing I’ve read all year. I’m Indian, and I’ve had two blood transfusions in my life - both during pregnancy. No one asked me a single question. No one checked for IgA. No one even knew what it was. What if I had it? What if I’d developed antibodies? I could’ve died silently in a hospital bed while nurses laughed about their weekend plans.
I’m not exaggerating. My cousin’s sister died after a transfusion. They thought it was an allergic reaction. Turned out she had IgA deficiency. They never tested. Never asked. Just assumed. Now I carry a laminated card in my purse. I hand it to every nurse. I don’t care if they roll their eyes. I’d rather be annoying than dead.
And yes, I know this is a niche issue. But if you don’t care about one person dying because no one knew the right protocol, then you’re part of the problem.
So let me get this straight. You’re telling me that a genetic condition that affects 1 in 600 people, mostly asymptomatic, is now being treated like a ticking time bomb because of transfusions? And the solution is expensive, rare, and unreliable blood products?
Also, why is this even a thing? Why not just screen every transfusion recipient? It’s cheaper than the drama. And why is recombinant IgA only available to 12 people? Sounds like a pharma scam. Someone’s sitting on a patent and letting people die to keep prices high.
I’m not saying this isn’t real. I’m saying the system is broken. And this post reads like a PSA written by someone who got paid by a blood bank.
As someone who’s had a few surgeries and needed blood, I’m shaking reading this. I had no idea. I thought transfusions were just… you know, blood. Like, pouring it in. No extra steps.
I’m going to call my doctor tomorrow and ask if I should get tested. I’ve had weird allergies and chronic sinus stuff for years. Could this be why? I’m not even mad - I’m just grateful I found this.
Also, I just ordered a medical bracelet. I’m putting it on my wrist like I’m in a superhero movie. "IgA Deficient - Washed Blood Only." I’m gonna wear it to the gym. Let’s make this a thing.
This is one of those posts that makes you feel like you’ve been living in a simulation where the rules were quietly rewritten while you weren’t looking.
IgA is basically the bouncer at the club of your mucous membranes. No bouncer? Anyone can walk in. Flu, parasites, gluten - all just chillin’ like they own the place.
But then transfusion? That’s like inviting a whole army of IgA into your body… and your immune system, which has been training for years to kill IgA, goes full Terminator. "TARGET ACQUIRED. ELIMINATE."
The fact that we’re still using 1970s protocols for this? Unacceptable. We’ve got CRISPR and AI and self-driving cars - but you still can’t get safe blood without a 72-hour wait and a prayer?
I’m not just impressed. I’m furious. And I’m telling everyone I know.
I just read this to my husband and he started crying. He’s had two transfusions after his heart surgery. He didn’t know he had IgA deficiency until last year. His doctor said, "Oh, that’s common." And then never mentioned the risk.
He’s fine now. But I’m so angry. We’re lucky he didn’t die. I’m going to make sure every doctor he sees gets a printed copy of this. I’m even going to email the hospital’s patient safety office.
You’re not just sharing info. You’re saving lives. Thank you.
I have IgA deficiency. I didn’t know until I was 32. I’d had three surgeries, two colds that turned to pneumonia, and one bout of giardia that lasted 11 months. No one connected the dots.
I’m now on a lifelong mission to educate. I’ve talked to nurses, ER staff, even my dentist. I carry my card. I wear my bracelet. I’ve sent this post to three friends who’ve had transfusions.
You’re not alone. And you’re not weird. You’re just one step ahead of a system that forgot you existed.
Why are we even talking about this like it’s a mystery? This is a global health failure. In India, we don’t even have standardized blood screening. People die every day because hospitals don’t have the resources to test for rare conditions.
And now you’re telling me the solution is expensive, imported, rare blood products? Who’s paying for that? The poor? The uninsured? The marginalized?
This isn’t science. This is privilege. If you’re rich, you get washed blood. If you’re not? You get lucky.
Stop pretending this is about medical awareness. It’s about inequality.