Indomethacin for Chronic Pain: What You Need to Know

Indomethacin isn’t the first drug people think of when they hear "chronic pain." You’ve probably heard of ibuprofen or naproxen more often. But for some types of long-term pain-especially those tied to inflammation-indomethacin can make a real difference. It’s not a miracle cure, and it’s not for everyone. But if you’ve tried other options and still struggle with joint pain, gout flares, or certain types of arthritis, it might be worth talking to your doctor about.
What is indomethacin?
Indomethacin is a nonsteroidal anti-inflammatory drug, or NSAID. That means it works by blocking enzymes in your body called COX-1 and COX-2, which produce chemicals that cause pain, swelling, and fever. It’s been around since the 1960s, originally developed to treat rheumatoid arthritis. Today, it’s still used for similar conditions, but also for gout, bursitis, tendonitis, and even some rare inflammatory disorders like ankylosing spondylitis.
Unlike over-the-counter NSAIDs, indomethacin is only available by prescription in the U.S. and most other countries. That’s because it’s stronger-and carries more risks-than common painkillers like Advil or Aleve. The typical starting dose for chronic pain is 25 mg two or three times a day, sometimes increased to 50 mg depending on how your body responds. It comes in capsules, oral suspensions, and suppositories, which helps if you have trouble swallowing pills.
How it works for chronic pain
Chronic pain isn’t just "feeling sore" for months. It’s often caused by ongoing inflammation. That’s where indomethacin steps in. For example, if you have gout, uric acid crystals build up in your joints and trigger a fierce inflammatory response. Indomethacin can shut that down fast, often reducing pain within hours. In one 2021 clinical review, patients with acute gout attacks reported up to 70% pain reduction within 24 to 48 hours of taking indomethacin.
It’s also used for osteoarthritis and rheumatoid arthritis when other NSAIDs don’t cut it. Some patients with chronic back pain from spinal inflammation find relief with indomethacin where celecoxib or diclofenac didn’t help. That’s because indomethacin is more potent at suppressing certain inflammatory pathways, especially those linked to prostaglandin E2, a key player in joint pain.
But here’s the catch: it doesn’t fix the root cause. It doesn’t repair damaged cartilage or stop autoimmune attacks. It just turns down the volume on the pain signal. That’s why it’s often used alongside physical therapy, weight management, or disease-modifying drugs.
Who benefits most?
Not everyone with chronic pain will respond to indomethacin. It works best for inflammatory types of pain, not nerve pain or muscle spasms. Here are the conditions where it’s most commonly prescribed:
- Gout: Especially for acute flares. It’s often preferred over colchicine when kidney function is normal.
- Rheumatoid arthritis: When symptoms are severe and other NSAIDs fail.
- Ankylosing spondylitis: A type of arthritis affecting the spine. Studies show indomethacin reduces stiffness and improves mobility better than placebo.
- Bursitis and tendonitis: Especially around the shoulder, hip, or elbow.
- Pseudogout: Similar to gout but caused by calcium crystals.
If your pain comes from fibromyalgia, neuropathy, or chronic headaches, indomethacin is unlikely to help. Those conditions need different approaches-like antidepressants, anticonvulsants, or nerve blocks.
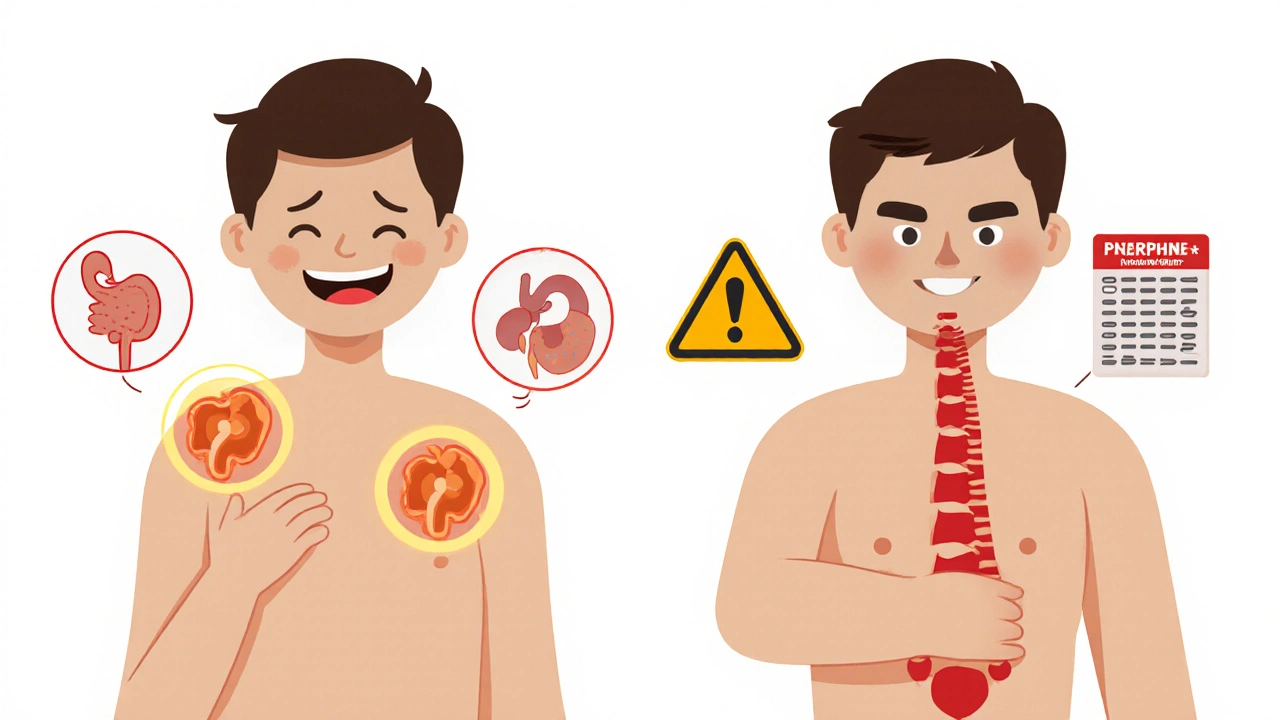
The risks you can’t ignore
Indomethacin isn’t gentle. It’s one of the most likely NSAIDs to cause side effects. The most common ones include stomach upset, nausea, dizziness, and headaches. But the serious ones? They’re why doctors don’t hand this out like candy.
- Stomach ulcers and bleeding: Risk is 3 to 5 times higher than with ibuprofen. People over 65, those on blood thinners, or with a history of ulcers should avoid it unless closely monitored.
- Kidney damage: It reduces blood flow to the kidneys. If you’re dehydrated, have heart failure, or already have kidney disease, this can make things worse.
- High blood pressure: NSAIDs can raise blood pressure, and indomethacin is among the worst offenders. If you’re on hypertension meds, your doctor will need to check your numbers more often.
- Heart risks: Like other NSAIDs, long-term use may increase heart attack or stroke risk, especially in people with existing heart disease.
One study published in Arthritis & Rheumatology in 2023 found that patients taking indomethacin daily for over six months had a 40% higher chance of gastrointestinal complications compared to those on naproxen. That’s not a small number.
Because of this, doctors usually start low and go slow. They’ll often prescribe a proton pump inhibitor like omeprazole at the same time to protect your stomach. They’ll also check your kidney function and blood pressure before and during treatment.
How it compares to other NSAIDs
| Drug | Strength | GI Risk | Kidney Risk | Best For |
|---|---|---|---|---|
| Indomethacin | High | Very High | High | Gout, ankylosing spondylitis, severe arthritis |
| Naproxen | Medium | Medium | Medium | Osteoarthritis, general inflammation |
| Diclofenac | High | High | Medium | Joint pain, tendonitis |
| Celecoxib (Celebrex) | Medium | Low | Low | Patients with stomach history |
| Ibuprofen | Low | Low | Low | Mild to moderate pain |
As you can see, indomethacin is the strongest on the list-but also the riskiest. That’s why it’s usually a second- or third-line option. If naproxen or diclofenac doesn’t work, then your doctor might consider indomethacin. If you’ve had stomach bleeding before, celecoxib is safer. If you’re just starting out, ibuprofen is the go-to.
What to expect when you start taking it
If your doctor prescribes indomethacin, you’ll likely begin with 25 mg two or three times a day. You should take it with food or milk to reduce stomach upset. Don’t lie down for at least 10 minutes after taking it.
Most people notice pain relief within 24 to 48 hours. If you’re using it for gout, you might feel better faster-sometimes even within 12 hours. But if you don’t notice improvement after a week, it’s probably not going to work for you. That’s not a sign you need a higher dose; it’s a sign you need a different treatment.
Your doctor will probably schedule a follow-up in 2 to 4 weeks. They’ll check your blood pressure, ask about stomach symptoms, and may order a basic blood test to check kidney function and liver enzymes. If everything looks good, they might keep you on it. If not, they’ll switch you to something else.
Don’t stop taking it suddenly if you’ve been on it for more than a few weeks. That can cause rebound inflammation or increased pain. Always taper off under medical supervision.
When not to use indomethacin
There are clear red flags. Avoid indomethacin if you:
- Have had a previous allergic reaction to aspirin or other NSAIDs
- Are in your third trimester of pregnancy
- Have active peptic ulcer disease or gastrointestinal bleeding
- Have severe heart failure or kidney disease
- Are taking blood thinners like warfarin or apixaban
- Are over 75 and have no prior experience with NSAIDs
Also, don’t mix it with other NSAIDs-not even aspirin. That doubles your risk of bleeding and kidney damage. Even herbal supplements like ginger or turmeric can increase bleeding risk, so tell your doctor about everything you’re taking.

Long-term use: Is it safe?
Indomethacin was never designed to be a lifelong medication. It’s meant for short-term control of flare-ups. But some people with chronic conditions like ankylosing spondylitis use it for years. That’s not ideal, but sometimes it’s necessary.
Long-term users need regular monitoring: every 3 to 6 months for blood pressure, kidney function, and liver tests. They should also be screened for signs of anemia or hidden stomach bleeding. If you’re on it long-term, ask your doctor about adding a proton pump inhibitor permanently.
There’s no hard rule that says you can’t take it for 5 or 10 years-but the longer you take it, the more likely you are to face complications. Many doctors will try to wean patients off it over time, especially if newer biologic drugs (like TNF inhibitors) become available.
Alternatives if indomethacin doesn’t work or isn’t safe
If indomethacin isn’t helping-or if the side effects are too much-there are other paths:
- Physical therapy: Especially for spine or joint pain. Movement can reduce inflammation naturally.
- Corticosteroid injections: For localized pain like bursitis or tendonitis. One shot can last months.
- Biologics: For autoimmune arthritis like rheumatoid or ankylosing spondylitis. Drugs like adalimumab or etanercept target the immune system directly.
- Acetaminophen: For mild pain without inflammation. Safer for the stomach and kidneys, but doesn’t reduce swelling.
- Topical NSAIDs: Gels or patches with diclofenac or ketoprofen. They deliver pain relief with far less systemic risk.
Some patients also find relief with heat therapy, acupuncture, or mindfulness-based stress reduction. These don’t replace medication, but they can reduce how much you need.
Final thoughts
Indomethacin is a powerful tool-but only for the right kind of pain. If you have inflammatory arthritis, gout, or tendonitis that hasn’t responded to milder drugs, it could be the breakthrough you’ve been waiting for. But if you’re looking for a quick fix for general aches, or if you’ve got stomach, kidney, or heart issues, it’s not worth the risk.
The key is working with your doctor to weigh the benefits against the dangers. Don’t assume it’s just another pain pill. It’s not. It’s a strong medicine with real consequences. But when used carefully, it can give people back their mobility, their sleep, and their quality of life.
Can indomethacin be used for back pain?
Yes-but only if the back pain is caused by inflammation, like ankylosing spondylitis or severe arthritis in the spine. It won’t help with muscle strains, herniated discs, or nerve-related pain. Your doctor can help determine the source of your pain before prescribing it.
How long does it take for indomethacin to work?
For acute conditions like gout, many people feel relief within 12 to 48 hours. For chronic conditions like arthritis, it may take a few days to a week to notice consistent improvement. If there’s no change after 7 days, it’s unlikely to work for you.
Is indomethacin stronger than ibuprofen?
Yes, significantly. Indomethacin is about 10 times more potent than ibuprofen in reducing inflammation. That’s why it’s prescribed for severe cases where ibuprofen doesn’t help. But this also means it carries a much higher risk of side effects.
Can I drink alcohol while taking indomethacin?
No. Alcohol increases your risk of stomach bleeding and liver damage when combined with indomethacin. Even one drink a day can be dangerous. It’s best to avoid alcohol entirely while on this medication.
Does indomethacin cause weight gain?
Not directly. But indomethacin can cause fluid retention, which may lead to temporary swelling or a slight increase on the scale. If you notice sudden weight gain, swelling in your legs, or shortness of breath, contact your doctor-it could be a sign of heart or kidney problems.
Is there a generic version of indomethacin?
Yes. Indomethacin is available as a generic drug, and it’s much cheaper than brand-name versions like Indocin. The generic is just as effective and is covered by most insurance plans.

15 Comments
Indomethacin saved my life when nothing else did. I had ankylosing spondylitis so bad I couldn’t tie my shoes. Took me six months to find a doc who’d even consider it. Now? I hike, I dance, I play with my nephews. Yeah, I take omeprazole like it’s candy and get blood work every three months. But I’d rather live with monitoring than live in a wheelchair. Don’t let the scary side effects scare you off if you’ve got real inflammatory pain. This ain’t ibuprofen. It’s a sledgehammer-and sometimes you need a sledgehammer.
Look, I get it. Indomethacin’s the Hulk of NSAIDs. But I’ve seen too many people on it who thought they were ‘tough’ and ignored the stomach warnings. One buddy took it for 18 months without PPIs. Ended up with a perforated ulcer. Got a colostomy bag at 42. I’m not saying don’t use it-I’m saying don’t be dumb. Your doctor didn’t give you this because they like you. They gave it to you because you’ve already tried everything else. Treat it like a loaded gun. Not a vitamin.
It doesn’t work for back pain unless it’s inflammatory. Duh.
Wow. So we’re just gonna ignore the fact that this drug is basically a slow-motion suicide pill for people over 60? I mean, I get it-your cousin’s cousin had gout and it worked. But the FDA should’ve banned this decades ago. It’s like prescribing cyanide with a side of aspirin. And don’t even get me started on the ‘it’s just a pill’ crowd. You think your kidneys are invincible? You’re not 25 anymore. Wake up.
It is interesting to note that indomethacin’s potency stems from its non-selective COX inhibition, which distinguishes it from COX-2-specific agents like celecoxib. The pharmacokinetic profile, particularly its half-life of 2–4 hours, necessitates multiple daily dosing, which may contribute to poor adherence in elderly populations. Furthermore, its association with elevated serum creatinine levels in longitudinal studies suggests a need for more rigorous renal monitoring than is currently standard in primary care. One wonders whether the clinical utility justifies the resource burden of surveillance.
Been on it for 3 years. 🤕💊 Still walking. Still working. Still alive. My doc checks my kidneys every 90 days. I drink water like it’s my job. I take my PPI like it’s my religion. It’s not perfect. But it’s better than crying in the shower every morning. 🙏
Let’s be real-indomethacin is the punk rock of NSAIDs. Loud, dangerous, and kinda beautiful when it hits right. I’ve seen people go from wheelchair to walking stick to hiking boots on this stuff. But man, you gotta treat it like a wild animal. No alcohol. No other NSAIDs. No ‘I’ll just take one more today.’ You don’t outsmart this drug. You partner with it. And if your doc isn’t talking about PPIs, kidney tests, and blood pressure? Find a new doc. This ain’t a ‘take as needed’ situation. It’s a ‘I’m serious about your life’ situation.
They say ‘it doesn’t fix the root cause.’ But isn’t that the whole point of pain management? We don’t fix broken hips with ibuprofen-we fix the pain so you can fix the hip. Indomethacin isn’t a cure. It’s a bridge. And if you’re stuck on the other side of chronic inflammation, bridges are kind of the whole damn point. Stop looking for miracles. Look for relief. And if you get it? Take the damn pill.
As a British physician with over two decades of clinical experience, I must emphasize that the American medical community’s cavalier attitude toward indomethacin is nothing short of alarming. In the NHS, we reserve this agent for tertiary care settings only, under rheumatology supervision, with mandatory fortnightly monitoring. The notion that a patient might self-prescribe or ‘trial’ this drug is not merely irresponsible-it is tantamount to medical negligence. The UK has a lower incidence of NSAID-induced GI bleeds precisely because we do not treat this as a ‘second-line option’-we treat it as a last-resort weapon.
Wait, wait, wait-so you’re telling me this thing is 10x stronger than ibuprofen? And you’re telling me to take it with food? And not lie down? And get blood work? And avoid alcohol? And take a stomach pill? And not use it if you’re over 75? And check kidney function? And it’s only for inflammatory pain? So… why is this even on the market? Why not just give us a checklist and a warning label that says ‘DO NOT USE UNLESS YOU’RE A MEDICAL GENIUS WITH A TEAM OF NURSES’? I’m just asking.
indomethicin? i think you mean indomethicin. anyway, my uncle took it and got a heart attack. so yeah. no thanks. also, the whole 'inflammatory pain' thing is just a scam. pain is pain. you just wanna sell more drugs.
Of course it works. It’s a steroid in disguise. You think the FDA just lets this out because it’s safe? They’re not stupid. They know it’s a sledgehammer. But they let it stay because the pharmaceutical lobby owns them. You think your doctor really cares? They get a kickback every time they prescribe it. Read the studies. The GI risk? It’s not 3–5x higher. It’s 8x. And they don’t tell you that. They just say ‘take it with food.’
Let’s break this down statistically. The 40% increased GI complication rate over naproxen? That’s a hazard ratio of 1.4. With a 95% CI of 1.2–1.6. That’s not ‘dangerous’-that’s statistically significant but clinically marginal for a 45-year-old with no comorbidities. Meanwhile, the pain relief is a Cohen’s d of 1.2. That’s massive. So yes, it’s riskier. But risk isn’t binary. It’s a trade-off. And if your pain is a 9/10 and your quality of life is 2/10? The math is clear. Stop moralizing. Start calculating.
I was on this for 6 months. My knees felt like they were made of butter. I could walk to the mailbox without crying. Then I got a stomach bleed. They said it was ‘unavoidable.’ I said, ‘I trusted you.’ Now I’m on biologics. I lost my job. My husband left. My dog won’t look at me. I still take indomethacin sometimes. Just… on the weekends. When I’m alone. And I cry while I swallow it. And I don’t tell anyone. Because I’m weak. And I’m scared. And I’m tired.
indomethacin is a government mind control drug disguised as pain relief. they want you dependent so you cant think straight. the kidney warnings? fake. the ulcers? a cover. the real reason? it suppresses your aura. they dont want you feeling too good. you think your pain is from arthritis? no. its from the chemtrails. and this pill makes it worse. i stopped taking it. now i eat cayenne pepper and meditate under my bed. i feel 100% better. the system is scared of me now. they sent 3 vans to my house. they want me back in the system.