Lithium Interactions: NSAIDs, Diuretics, and Dehydration Risks

When you take lithium for bipolar disorder, even small changes in your body can push your lithium levels into dangerous territory. This isn't just a theoretical risk - it's a real, life-threatening issue that happens more often than most people realize. Lithium has a narrow therapeutic window: the difference between a helpful dose and a toxic one is tiny. Levels between 0.6 and 1.2 mmol/L are safe. Go above that, and you risk confusion, tremors, seizures, or even death. And the biggest culprits aren't mysterious drugs - they're everyday medications and habits you might not even think twice about.
How Lithium Works - and Why It's So Fragile
Lithium doesn't get broken down by your liver. Instead, nearly 95% of it leaves your body through your kidneys. That means anything that affects kidney function - or how much fluid and salt you have in your blood - directly changes how much lithium stays in your system. It's not complicated, but it's incredibly sensitive. A little less water, a little less salt, or a common painkiller can cause lithium to build up like a clogged drain.
That’s why even people who’ve been on lithium for years without problems can suddenly crash into toxicity. It’s not about the lithium dose. It’s about what else is happening in your body.
NSAIDs: The Silent Lithium Boosters
Non-steroidal anti-inflammatory drugs - think ibuprofen, naproxen, diclofenac - are the most common offenders. People take them for headaches, back pain, arthritis. But when you add them to lithium, your kidneys slow down how fast they clear lithium. Why? NSAIDs block prostaglandins, chemicals your kidneys use to keep blood flowing normally. Less blood flow = less lithium filtered out.
The effect isn’t subtle. Studies show NSAIDs can raise lithium levels by 25% to 60%, depending on the drug. Indomethacin? That one can spike levels by up to 60%. Ibuprofen? Still a 25-40% jump. Celecoxib? A bit milder, but still risky. And here’s the kicker: this doesn’t take weeks. The rise in lithium levels often starts within the first week of taking the NSAID. If you’re over 65, have kidney issues, or are dehydrated? Your risk triples.
There’s a documented case in New Zealand of a 72-year-old woman who died from lithium toxicity after starting an NSAID. She was on lithium, an ACE inhibitor for blood pressure, and then took ibuprofen for joint pain. Her lithium levels weren’t checked for months. She never had a chance.
Diuretics: A Double-Edged Sword
Diuretics - water pills - are another major problem. But not all of them are equal. Thiazide diuretics like hydrochlorothiazide (HCTZ) are the worst. They cause lithium levels to jump 25-50% within 7-10 days. Why? Thiazides make your kidneys reabsorb more sodium. And lithium? It rides along with sodium. More sodium reabsorption = more lithium stuck in your blood.
Loop diuretics like furosemide are less dangerous, but still risky. They raise lithium levels by 10-25%. That’s still enough to cause problems, especially if you’re already borderline. And then there are the oddballs: osmotic diuretics like mannitol and carbonic anhydrase inhibitors like acetazolamide. These actually lower lithium levels by 15-30%. That’s a different kind of danger - you might think your mood is under control, but your lithium level has dropped too low.
And don’t forget herbal diuretics. Those “natural” weight-loss teas or supplements? They’re not safe either. They work by flushing out water - and that dehydration can push lithium levels up by 15-25% on its own. No prescription needed. No warning label. Just a dangerous cocktail.
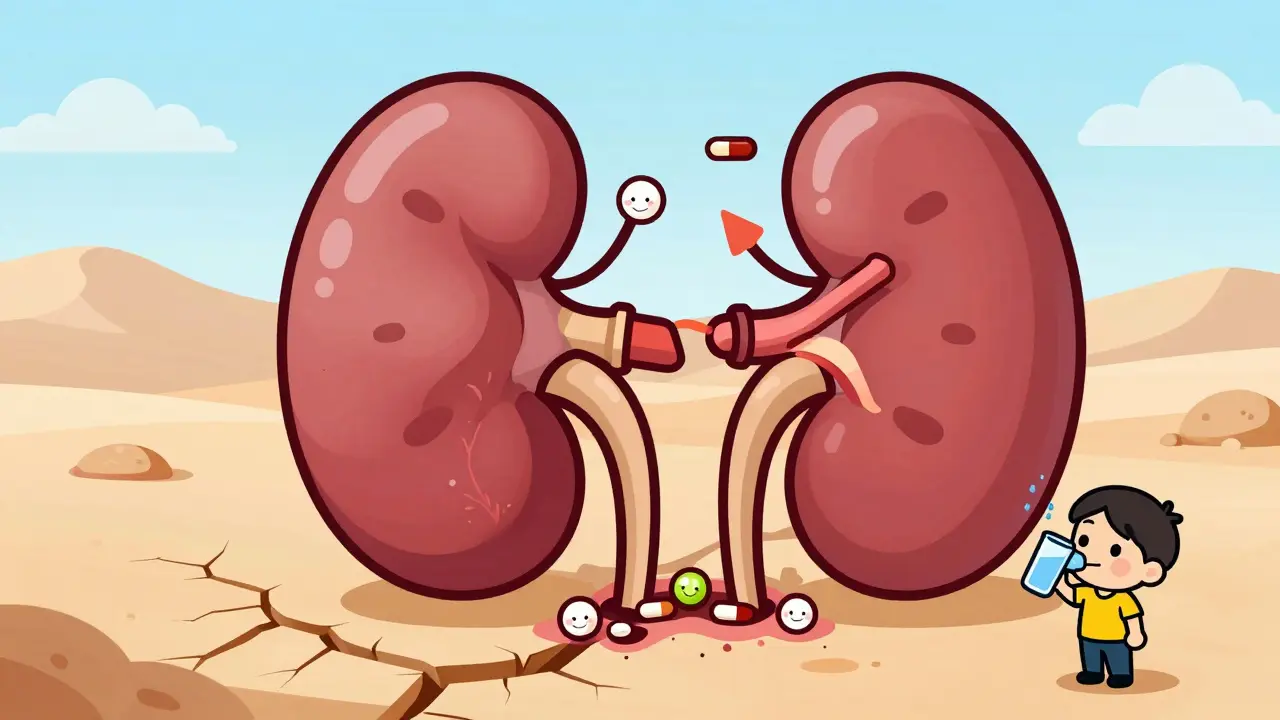
Dehydration: The Hidden Trigger
You don’t need to be on a drug to be at risk. Just being mildly dehydrated can be enough. Losing as little as 2-3% of your body weight in water - think a hot day, a long flight, vomiting, or diarrhea - can raise lithium levels by 15-25%. Your kidneys start conserving sodium. Lithium follows. Boom. Toxicity.
And it’s not just about drinking less water. It’s about salt. If you suddenly eat less salt - say, you’re on a low-sodium diet for heart health - lithium levels climb. More salt? Lithium levels drop. A change of just 20-30 mmol of sodium per day can shift your lithium level by 10-20%. That’s why doctors tell you to keep your salt intake steady. Not too high. Not too low. Just right.
Travelers are especially vulnerable. Flying long distances, sweating in hot climates, or getting sick on vacation? All of those things can trigger lithium toxicity. One study found that people traveling to tropical areas were at high risk because of heat, reduced fluid intake, and stomach bugs. No one warned them. They just thought they were fine.
Who’s Most at Risk?
This isn’t a risk that affects everyone equally. Certain people are sitting on a ticking time bomb:
- People over 65: Their kidneys don’t filter as well. They’re 3.2 times more likely to develop lithium toxicity.
- Those with kidney disease: Even mild chronic kidney disease makes lithium clearance drop.
- People with heart failure: Fluid retention and medications for heart issues compound the problem.
- Anyone on multiple interacting drugs: NSAID + thiazide + ACE inhibitor? That’s a perfect storm.
And here’s the scary part: many of these people aren’t told. They’re given an NSAID for arthritis without anyone checking their lithium level. Or they’re told to cut salt for blood pressure, without realizing it could make their mood meds stop working - or turn toxic.
What to Do - And What Not to Do
If you’re on lithium, here’s what you need to know:
- Avoid NSAIDs if you can. Use acetaminophen (Tylenol) for pain instead. It doesn’t interfere with lithium.
- Never start a diuretic without telling your doctor. If you’re on HCTZ for high blood pressure, ask if there’s a safer alternative.
- Drink water - but don’t overdo it. Aim for consistent hydration. No crash drinking. No going dry for days.
- Keep your salt intake steady. Don’t suddenly go low-sodium or high-sodium. Consistency matters more than perfection.
- Get your lithium level checked. If you start any new medication - even an OTC one - get your lithium checked within 5-7 days. And keep checking weekly for the first month.
- Know the early signs. Diarrhea, drowsiness, lightheadedness, hand tremors, nausea. These aren’t just “bugs.” They’re warning signs. Call your doctor immediately if they show up.
And if your doctor says it’s okay to take an NSAID? Make sure they’ve checked your kidney function, adjusted your lithium dose, and set up a monitoring plan. Don’t assume they know. Ask.
The Bottom Line
Lithium is one of the most effective mood stabilizers we have. But it’s also one of the most dangerous if you don’t treat it like the precision tool it is. The interactions with NSAIDs, diuretics, and dehydration aren’t rare. They’re predictable. Avoidable. Preventable.
It’s not about fear. It’s about awareness. A simple change in your daily routine - skipping the ibuprofen, drinking water on a flight, keeping your salt intake steady - can keep you safe. You don’t need to live in fear. But you do need to be informed.
If you’ve been on lithium for years and never had a problem, that doesn’t mean you’re immune. It just means you haven’t hit the trigger yet. And that trigger can come from anywhere.
Can I take ibuprofen while on lithium?
It’s not recommended. Ibuprofen can raise lithium levels by 25-40%, increasing the risk of toxicity. If you must take it, get your lithium level checked within a week and monitor for symptoms like nausea, tremors, or confusion. Acetaminophen (Tylenol) is a safer pain relief option.
Do all diuretics raise lithium levels?
No. Thiazide diuretics like hydrochlorothiazide are the biggest risk - they can raise lithium by 25-50%. Loop diuretics like furosemide raise levels less (10-25%). But osmotic diuretics (mannitol) and carbonic anhydrase inhibitors (acetazolamide) actually lower lithium levels. Always check with your doctor before starting any new diuretic.
How much water should I drink if I’m on lithium?
Drink enough to keep your urine pale yellow - about 8-10 cups daily, unless your doctor says otherwise. Don’t restrict fluids, especially during heat, illness, or travel. Mild dehydration (just 2-3% fluid loss) can spike lithium levels by 15-25%.
Can changing my salt intake affect lithium?
Yes. Eating less salt can raise lithium levels by 10-20%. Eating more salt can lower them. The key is consistency. Don’t suddenly go low-sodium or binge on salty foods. Stick to your usual intake - your lithium level depends on stable sodium levels in your blood.
What are the first signs of lithium toxicity?
Early signs include diarrhea (68% of cases), drowsiness (47%), lightheadedness (52%), and hand tremors. Later signs include blurred vision, ringing in the ears, confusion, or muscle weakness. If you notice any of these, stop taking NSAIDs or diuretics, drink water, and contact your doctor immediately.
Should I avoid travel if I’m on lithium?
No - but be prepared. Travel, especially to hot climates or on long flights, increases dehydration risk. Pack extra water, avoid alcohol, carry a note from your doctor about your lithium use, and check your lithium level before and after long trips. Many people travel safely - they just plan ahead.
How often should lithium levels be checked?
If you’re stable, every 3-6 months is typical. But if you start a new medication, change your diet, get sick, or travel, check within 5-7 days and again at 2-4 weeks. After adding an NSAID or diuretic, weekly checks for the first month are standard practice.

9 Comments
Man, I’ve been on lithium for 12 years and never thought about how fragile this stuff is. I mean, I take ibuprofen like it’s candy when my back flares up. Guess I’ve been playing Russian roulette with my brain. This post laid it out like a knife to the throat - no fluff, no sugar. I’m switching to Tylenol tomorrow. No debate. Also, I’ve been cutting salt ‘cause my doc said ‘heart healthy’ - turns out that might’ve been the quiet killer. Holy shit. I’m getting my levels checked next week. Thanks for the wake-up call.
You people are so naive. This isn’t just about ‘being careful’ - it’s corporate malpractice. Big Pharma doesn’t want you to know how dangerous lithium is because they’d have to redesign the entire mental health system. NSAIDs? Diuretics? They’re not ‘accidental’ interactions - they’re engineered loopholes. Doctors get paid to prescribe them. You think your doctor cares? They’re paid per script. Your life is a line item in their bonus spreadsheet. Wake up. This system is built to keep you dependent - not healthy.
Let’s examine the pharmacokinetics with scientific rigor. Lithium, being a monovalent cation, exhibits near-complete renal excretion - approximately 95% - via glomerular filtration and tubular reabsorption. The nephron’s sodium-lithium competition at the distal convoluted tubule is the critical nexus. NSAIDs inhibit cyclooxygenase-1 and -2, thereby reducing prostaglandin E2 synthesis, which normally maintains renal perfusion pressure. This results in afferent arteriolar vasoconstriction, decreased glomerular filtration rate (GFR), and consequent lithium retention. Thiazide diuretics, by blocking the Na-Cl cotransporter, increase sodium reabsorption - and lithium, due to its ionic mimicry, co-reabsorbs. The magnitude of elevation correlates with sodium depletion magnitude. This is not anecdotal - it’s biochemistry. And yet, the medical community continues to under-educate patients. The data is clear. The protocol is established. The negligence is systemic.
Okay, I’m a nurse and this is so on point. I’ve seen two patients in the last year crash into lithium toxicity after starting HCTZ for hypertension - both were asymptomatic until they came in with tremors and confusion. One had just returned from a 14-hour flight and didn’t drink water. The other was on a ‘low-sodium diet’ for ‘heart health’ and cut salt completely. Both had their levels checked months ago - no one thought to recheck after new meds or lifestyle changes. I wish more patients knew: lithium isn’t like SSRIs. It’s more like warfarin - tiny changes, huge consequences. Please, if you’re on it, track your sodium and fluids like your life depends on it - because it does.
Real talk: I’ve been on lithium for 8 years. I drink water like it’s my job. I keep my salt steady. I use Tylenol. I check my levels every 4 months. But I never knew how much travel messed with it. Last year I went to Mexico - 100-degree heat, no AC on the flight, got a stomach bug. Came home feeling like a zombie. Thought I was just jet-lagged. Turns out my lithium was at 1.4. I was one step from the ICU. Now I carry a little card in my wallet that says ‘Lithium Patient - Avoid NSAIDs, Diuretics, Dehydration.’ My doc didn’t give it to me. I made it myself. Simple. Life-saving.
My sister’s on lithium. She’s 68. Had a stroke last year. Now she’s on a diuretic for fluid retention. I was terrified. I dug into this stuff. Found out HCTZ is a nightmare combo. We switched her to a different BP med - spironolactone, actually. It’s potassium-sparing, so it doesn’t mess with lithium like thiazides do. She’s been stable for 6 months now. I wish more families knew this. It’s not just the patient - it’s the whole support system. Talk to your doctor. Ask questions. Don’t assume. I’ve learned so much from this. Thank you for writing this.
oh my gosh. i didn't even realize that dehydration could do this. i was just like, 'oh i'm gonna drink less water on my hike' and now i'm like... wait. did i almost kill myself? i've been on lithium for 5 years and never had an issue. but now i'm terrified. i'm gonna start carrying a water bottle everywhere. and i'm throwing out my ibuprofen. i didn't even know tylenol was the safe option. i thought all painkillers were the same. i'm so grateful for this post. i'm gonna print it out and give it to my mom. she's on lithium too. she thinks she's fine. she's not. she needs to know. thank you.
Just to clarify a nuance: osmotic diuretics like mannitol and carbonic anhydrase inhibitors like acetazolamide reduce lithium levels via different mechanisms. Mannitol induces osmotic diuresis, which increases lithium excretion by reducing tubular reabsorption. Acetazolamide inhibits carbonic anhydrase in the proximal tubule, causing bicarbonate wasting and mild metabolic acidosis, which increases lithium clearance. These are clinically useful in cases of lithium overdose - sometimes used in ER settings. But for chronic users, they’re not replacements for hydration or sodium stability. The key takeaway? Lithium is a mineral that behaves like a salt. It’s not a drug - it’s a physiological variable. Treat it like your electrolyte balance depends on it - because it does.
Lithium toxicity? Please. It’s all a psyop. The real danger is the psychiatric-industrial complex pushing lithium because it’s cheap and keeps people docile. NSAIDs? Diuretics? Dehydration? Those are just convenient scapegoats. The truth? Lithium is a heavy metal. It’s toxic by design. They don’t care if you live - they care if you’re compliant. They don’t want you to know that lithium can be replaced with nutritional interventions - magnesium, omega-3s, vitamin D. They want you dependent. This whole post? It’s designed to make you afraid of every pill, every meal, every breath. Don’t fall for it. Your mind is yours. Not theirs.