Medications with a Narrow Therapeutic Index: Why Expired Drugs Can Be Dangerous

Some medications don’t just stop working after they expire-they can turn dangerous. This isn’t true for most pills in your medicine cabinet, but for a small group of critical drugs called narrow therapeutic index (NTI) medications, even a tiny drop in potency can mean the difference between life and death.
What Makes a Drug Have a Narrow Therapeutic Index?
NTI drugs are like walking a tightrope. The amount needed to treat your condition is almost the same as the amount that can hurt you. For example, warfarin, used to prevent blood clots, has a therapeutic range where your blood takes just the right amount of time to clot. Too little, and you risk a stroke or pulmonary embolism. Too much, and you could bleed internally. The gap between safe and toxic is razor-thin-often less than 20%.
The U.S. Food and Drug Administration defines NTI drugs as those where small changes in blood concentration can cause serious harm: hospitalization, disability, or death. This isn’t theoretical. In clinical practice, doctors adjust doses in increments as small as 0.5 mg for drugs like levothyroxine or 0.1 mg for digoxin. Even a 5% loss in potency after expiration can push you out of that safe zone.
Common NTI drugs include:
- Warfarin (anticoagulant)
- Lithium (for bipolar disorder)
- Digoxin (for heart failure)
- Phenytoin (for seizures)
- Carbamazepine (for epilepsy and nerve pain)
- Levothyroxine (for hypothyroidism)
- Ciclosporin (for organ transplant patients)
- Theophylline (for asthma)
These aren’t optional meds. They’re life-sustaining. And because their absorption and metabolism vary so much between people, even switching brands can require a dose adjustment. That’s why the FDA requires generic versions of these drugs to meet stricter bioequivalence standards-90% to 111% of the brand-name drug’s concentration, compared to the usual 80% to 125% for most medications.
Why Expiration Dates Matter More for NTI Drugs
Most pills are still safe and effective years after their expiration date. A 1985 FDA study found that 90% of medications retained potency for at least five years past their labeled date, if stored properly. But that’s not good enough for NTI drugs.
Let’s say your warfarin tablet loses 8% of its potency after expiration. That might sound minor. But if your target INR is 2.8, and you’re taking 5 mg daily, an 8% drop means you’re now getting the equivalent of 4.6 mg. That could drop your INR from 2.8 to 2.1-below the therapeutic range. For someone with a mechanical heart valve, that’s a red flag for clotting.
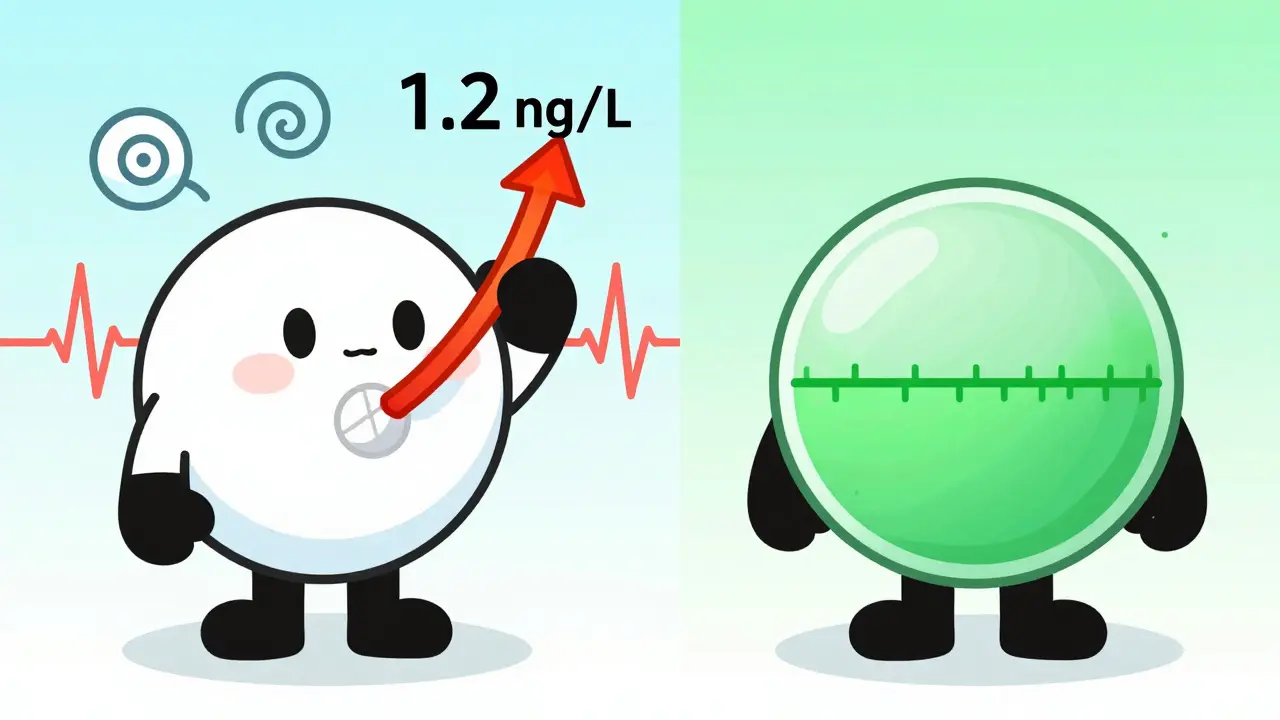
Or take digoxin. Its therapeutic range is 0.5 to 0.9 ng/mL. Toxicity starts above 1.2 ng/mL. That’s only a 33% increase from the top of the safe range to the bottom of the dangerous one. If degradation causes the concentration to rise even slightly-say, due to moisture exposure or heat-the drug can shift into toxicity. Symptoms like nausea, confusion, or irregular heartbeat can be mistaken for other illnesses, delaying treatment.
Some NTI drugs don’t just lose potency-they can form toxic breakdown products. While tetracycline is not an NTI drug, its degradation into a kidney-toxic compound is a warning sign. NTI drugs aren’t studied as thoroughly for post-expiration stability, but their narrow margins make any degradation unpredictable.
What Happens When You Take an Expired NTI Drug?
There are two real risks: underdosing and overdosing.
Underdosing: If the drug has degraded, you’re not getting enough. For someone on levothyroxine, that means fatigue, weight gain, depression, and eventually, heart problems. For a transplant patient on ciclosporin, it could mean organ rejection. These aren’t inconveniences-they’re medical emergencies.
Overdosing: Less common, but possible. Some formulations break down in ways that increase absorption or release the drug faster. A degraded phenytoin tablet might release its active ingredient unevenly, causing spikes in blood levels. That can lead to dizziness, slurred speech, or even seizures-the very condition it’s meant to prevent.
A 2014 study in the Journal of Clinical Pharmacy and Therapeutics found that drug-related problems involving NTI medications were far more likely to cause serious harm than those involving other drugs. And while no large studies have directly measured the effects of expired NTI drugs, the clinical evidence is clear: these drugs demand precision. Expired meds break that precision.
What Should You Do If You Find an Expired NTI Medication?
Don’t guess. Don’t take it. Don’t try to stretch it.
If you find an expired NTI drug:
- Stop using it immediately.
- Don’t refill it without talking to your doctor or pharmacist.
- Bring the expired bottle to your pharmacy for safe disposal.
- Ask your provider if you need a blood test to check levels before starting a new prescription.
For drugs like warfarin or lithium, your doctor may want to check your blood levels (INR or serum lithium) before and after switching to a new supply. Even if the new prescription looks the same, small differences in formulation or manufacturing can change how your body handles it.
Pharmacists are trained to flag NTI drugs. If you’re picking up a refill, ask: “Is this the same brand as before?” or “Should I get a blood test after starting this?” Most will know what you mean. If they don’t, it’s time to find a provider who does.
How to Avoid This Problem Before It Starts
Prevention is easier than fixing the fallout.
- Keep track of expiration dates. Put NTI meds in a separate bin or drawer. Set phone reminders 30 days before they expire.
- Don’t stockpile. Order only what you need for the next 30 to 60 days. Many NTI drugs come in 30-day supplies for a reason.
- Store them right. Keep them in a cool, dry place. Bathroom cabinets are terrible for humidity. A bedroom drawer or kitchen cabinet away from the stove is better.
- Ask about alternatives. Some NTI drugs have newer versions with more stable formulations. Talk to your doctor if you’re on an older version.
- Use one pharmacy. That way, your pharmacist can track all your meds and spot potential interactions or substitutions.
The Institute for Safe Medication Practices calls NTI drugs “high-alert medications.” That means they require extra care-like double-checking doses, using barcode scanners in hospitals, and avoiding substitutions without approval. You should treat your own supply the same way.

What’s Being Done to Improve Safety?
Regulators are slowly catching up. The FDA now requires replicate bioequivalence studies for four key NTI drugs: tacrolimus, phenytoin, levothyroxine, and carbamazepine. These studies test how consistently the drug performs in real patients-not just in a lab. That’s a big step forward.
Some manufacturers are now testing stability beyond the labeled expiration date for NTI drugs. A 2022 industry survey found 78% of major drugmakers conduct extended stability testing for these critical medications. But that data isn’t public. The expiration date on your bottle is still the only official guarantee.
Professional groups like the American Pharmacists Association are pushing for clearer labeling on NTI drugs-maybe even expiration dates printed in red or with a warning icon. Until then, the responsibility falls on you and your care team.
Bottom Line: When It Comes to NTI Drugs, Expired Means Unsafe
There’s no gray area. For medications like warfarin, lithium, or digoxin, expiration isn’t a suggestion-it’s a safety cutoff. These drugs don’t just lose effectiveness. They can become unpredictable, unreliable, or even harmful.
If you take one of these drugs, treat it like insulin or an EpiPen: if it’s expired, replace it. Don’t wait. Don’t ration. Don’t hope it’s still good. Your life depends on the dose being exact.
When in doubt, call your pharmacist. They’re your best line of defense. And if you’ve been using an expired NTI drug, tell your doctor. A simple blood test can catch a problem before it becomes a crisis.
These drugs save lives-but only when they work exactly as they should. And that’s only true when they’re fresh, stored right, and taken as prescribed.

11 Comments
so i took my warfarin from 2021 because ‘it’s just a pill’ and now my cat’s judging me harder than my pharmacist. thanks for the reminder, i’m replacing it today. also, my dog now barks at expiration dates. 🐶💊
Why are we even talking about this? In my day, people just took what was in the bottle and didn’t whine. You want precision? Go to Germany. We don’t need fancy labels to stay alive.
This is a critically important public health message. The pharmacokinetic variability of narrow therapeutic index medications demands rigorous adherence to expiration protocols. The clinical consequences of subtherapeutic or toxic dosing are not merely theoretical-they are documented, preventable, and tragically recurrent. Institutions must prioritize patient education on this issue, and regulatory bodies should consider mandatory color-coded labeling for NTI agents.
Let’s be real-most people don’t even know what ‘NTI’ stands for. I’ve seen folks take expired lithium because ‘it still looks fine.’ That’s not bravery, it’s Russian roulette with your brain chemistry. The FDA’s stricter bioequivalence standards for these drugs? Genius. Why isn’t this on every prescription bottle in neon green? Someone should make a meme: ‘Expired NTI meds: the silent killer your pharmacy doesn’t want you to know about.’
I work in a pharmacy, and I’ve seen it all. A man came in last week with his 3-year-old expired digoxin, saying, ‘My wife says it’s fine.’ I had to gently explain that her wife might be fine… but he wouldn’t be. We do free disposal bins, free blood-level check referrals, and we call patients 10 days before their NTI meds expire. It’s not just a job-it’s saving lives, one pill at a time. Please, if you’re on one of these, talk to your pharmacist. They’re not just handing out bottles-they’re holding your heartbeat in their hands.
Yeah. Expired meds are bad. Especially the important ones. Got it.
In my family, we’ve always kept a small log of medication expiration dates. My grandmother, who survived two heart surgeries, insisted on writing them in her journal next to her tea schedule. I still do it. It’s not paranoia-it’s ritual. And rituals, in medicine, are often the quietest form of survival.
Wow. Another ‘medical authority’ telling people what to do. Meanwhile, the real problem is Big Pharma’s profit-driven expiration dates. Why do you think they don’t test beyond 5 years? Because they want you buying more. This whole post is a marketing ploy disguised as science. Also, I’ve taken expired insulin for 12 years. Still alive. Your fear is not my reality.
My dad’s on warfarin. We throw out anything past the date. No questions.
My cousin in India take expired medicine all time. He say medicine is like tea, if you boil it long it still work. He live 80 year old with 12 medicine. Why you worry? You too much worry. You American too much worry.
It’s interesting how we treat expiration dates as absolute when, in reality, most drugs degrade gradually. But with NTI medications, that gradual shift becomes a cliff. Maybe the real question isn’t whether they’re still potent-but whether our medical system is designed to support the precision they require. We ask patients to be chemists, but we don’t give them the tools.