Red Flag Drug Combinations to Avoid for Safer Treatment

Every year, thousands of people die not from taking one drug too much, but from mixing two that seem harmless on their own. You might think taking your painkiller with a glass of wine is fine. Or that popping a Xanax after a long day won’t hurt if you’ve had a beer. But some combinations don’t just add risk-they multiply it. And the results can be deadly.
Why Mixing Drugs Is More Dangerous Than You Think
Drugs don’t just work alone. They talk to each other inside your body. When two or more substances enter your system at the same time, they can change how each one is absorbed, broken down, or affects your brain and organs. Sometimes they cancel each other out. More often, they team up to create something far worse. The most common killer combinations involve central nervous system (CNS) depressants. These include opioids like oxycodone, benzodiazepines like Xanax, alcohol, and even some sleep meds. All of them slow down your breathing and heart rate. When you mix them, your body doesn’t just get a little sleepy-it can stop breathing entirely.The Deadliest Pair: Opioids and Benzodiazepines
If you’re on a prescription painkiller like Vicodin or OxyContin, and your doctor also gave you Xanax or Valium for anxiety, you’re in a high-risk zone. The CDC found that in 2020, over 30% of opioid-related overdose deaths also involved benzodiazepines. That’s not a coincidence. It’s a pattern. These drugs work on the same part of your brain-the GABA system-that controls relaxation and breathing. Together, they push your system into deep sedation. Your breathing slows. Your heart rate drops. You might feel calm at first. Then you pass out. And if no one finds you, your body doesn’t wake up. Even if you’ve taken both drugs separately without issue, mixing them changes everything. The effect isn’t linear-it’s exponential. Two drinks and one pill might not seem like much. But together, they can be enough to stop your lungs from working.Alcohol + Opioids = Silent Killer
You might not think of alcohol as a drug, but it’s one of the most dangerous ones to mix with opioids. Alcohol enhances the sedative effect of painkillers, making dizziness, confusion, and nausea worse. But the real danger is respiratory depression-your brain forgets to tell your lungs to breathe. A study in the Journal of Clinical Pharmacology showed that combining alcohol with opioids increases the risk of respiratory failure by 4.5 times compared to using either alone. That’s not a small increase. That’s a red flag you can’t ignore. And it doesn’t take much. One or two drinks with a single dose of oxycodone has been enough to trigger respiratory arrest in people who had never overdosed before. A Reddit user shared how they went to the ER after just two beers with their prescribed pain meds after dental surgery. They needed naloxone to wake up. That’s not rare. It’s predictable.The Speedball: Cocaine and Heroin
This one’s called a “speedball” because it’s a push-pull on your body. Cocaine is a stimulant-it speeds up your heart, raises your blood pressure, and makes you feel energized. Heroin is a depressant-it slows everything down. People think they’re balancing each other out. They’re not. What actually happens is your heart is being torn in two directions. Your blood pressure spikes to dangerous levels-sometimes over 180/110. Your heart rate races between 110 and 160 beats per minute. Your brain gets flooded with dopamine, making it more addictive than either drug alone. And then there’s the crash. When the cocaine wears off, the heroin hits harder. Your breathing slows. Your heart struggles. Many high-profile deaths-from River Phoenix to Chris Farley-were linked to this combo. But it’s not just celebrities. It’s people in small towns, in apartments, in cars. All thinking they can handle it.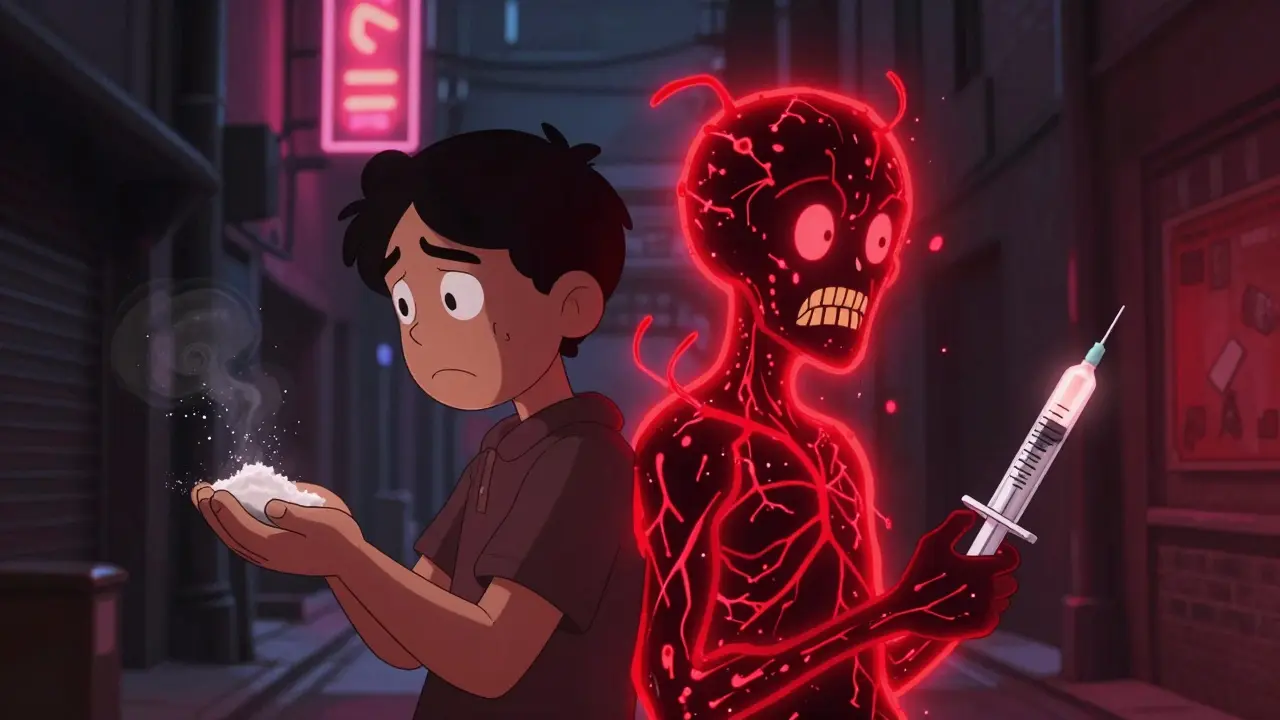
Alcohol + Cocaine = Cocaethylene, the Hidden Toxin
This combination creates a third substance your body didn’t ask for: cocaethylene. It’s made in your liver when alcohol and cocaine mix. It lasts longer than cocaine alone-up to 30 minutes more-and it’s 25% more likely to kill you. Cocaethylene doesn’t just raise your risk of heart attack. It damages your liver. Studies show that 65% of chronic users of this combo develop liver toxicity. It causes seizures, extreme stomach pain, and irregular heart rhythms. People who use this mix often don’t realize how much they’ve taken because the alcohol masks the high of cocaine. They keep going until their body gives out.Other Dangerous Combinations You Might Not Know About
You might not think antidepressants are risky, but some are. Mixing alcohol with venlafaxine (Effexor) lowers your tolerance for alcohol, meaning you can overdose on far less than you think. One study showed a 25% drop in the fatal alcohol threshold. Duloxetine (Cymbalta) and alcohol? That combo increases liver damage risk by 40%. Even if you’ve been drinking for years and never had a problem, adding this med can push your liver into failure. Buprenorphine, used to treat opioid addiction, becomes extremely dangerous with alcohol. It can cause your blood pressure to crash below 90/60, your breathing to slow to under 10 breaths per minute, and lead to coma. This isn’t theoretical. It’s happening in clinics and homes across the country.What You Can Do to Stay Safe
If you’re on any prescription medication, especially for pain, anxiety, or depression, ask your doctor or pharmacist: “Is it safe to drink alcohol with this?” Don’t assume it’s okay. Don’t rely on the label. Ask. If you’re using street drugs, know this: you don’t know what’s in them. The DEA says six out of ten fake pills now contain fentanyl. That means even one pill you think is oxycodone could be pure fentanyl. Add alcohol, benzodiazepines, or cocaine? The odds of survival drop fast. Use harm reduction tools. Naloxone kits are available for free in many places. They won’t help with benzodiazepines or alcohol overdoses, but they can reverse opioid overdoses-and they’ve been shown to cut overdose deaths by 22% in communities where they’re widely distributed.
Technology Is Helping-But You Still Need to Be Careful
Many pharmacies now use drug interaction checkers that flag dangerous combos before you even leave the counter. Medicare Part D plans have been required since 2019 to alert prescribers when someone is getting both opioids and benzodiazepines. That’s led to an 18% drop in dangerous co-prescribing. But tech doesn’t replace human judgment. If you’re mixing drugs because you’re self-medicating for anxiety, trauma, or pain, you need support-not just a warning. Talk to someone. Call a helpline. Reach out. You don’t have to do this alone.Final Warning: It’s Not Worth the Risk
There’s no safe way to mix opioids with alcohol, benzodiazepines, or stimulants. There’s no “just one” that won’t hurt. There’s no “I’ve done it before.” Your body changes. Your tolerance shifts. What was fine last month could kill you today. The goal isn’t to scare you. It’s to make you aware. Every year, people die because they didn’t know. Or because they thought they knew better. Don’t be one of them.Can I have one drink while taking my pain medication?
No. Even one drink can significantly increase the risk of respiratory depression, dizziness, and overdose when mixed with opioids or benzodiazepines. The interaction isn’t predictable-it doesn’t matter if you’ve done it before. Your body’s response can change without warning.
Are over-the-counter meds safe to mix with alcohol?
Not always. Many OTC pain relievers like acetaminophen (Tylenol) can cause severe liver damage when mixed with alcohol. Cold and allergy meds with antihistamines can cause extreme drowsiness. Always check the label or ask a pharmacist before combining anything with alcohol.
What should I do if someone overdoses on a drug combo?
Call 911 immediately. If the person is unconscious and you suspect opioids are involved, give naloxone if you have it. Even if you’re unsure, don’t wait. Keep them awake, on their side, and stay with them until help arrives. Time is critical.
Can I stop my anxiety meds if I want to drink?
Never stop taking prescribed meds without talking to your doctor. Suddenly stopping benzodiazepines or antidepressants can cause seizures, severe anxiety, or withdrawal. If you want to drink, talk to your provider about safer alternatives or a plan to taper off-don’t quit cold turkey.
Are there apps or tools to check drug interactions?
Yes. Tools like WebMD’s Drug Interaction Checker and Medscape’s Drug Interaction Checker are free and reliable. Enter all medications, supplements, and alcohol use. But remember: these tools don’t replace professional advice. Always confirm with your doctor or pharmacist.

10 Comments
So let me get this straight - taking a beer with my oxycodone is basically suicide, but chugging five energy drinks with Adderall is just ‘vibes’? Funny how the system picks its battles.
Oh, how delightful. Another performative public health PSA dressed up like a medical journal. Let me guess - you also think people who drink while on SSRIs are ‘moral failures’? The irony is thick enough to spread on toast. People aren’t dumb. They’re self-medicating because the system failed them. You want to save lives? Fix the mental health infrastructure. Don’t lecture us about wine and Xanax like we’re toddlers holding matches.
alcohol + painkillers = bad yeah but also like… how many people actually die from one drink and one pill? its not like everyone who does it drops dead. maybe chill with the fear mongering
What’s fascinating isn’t the pharmacology - it’s the cultural denial. We’ve normalized the ritual of self-annihilation through polypharmacy while pretending it’s ‘self-care.’ The GABA system isn’t a buffet. It’s a fragile cathedral, and we’re all swinging sledgehammers in it, hoping the stained glass won’t shatter. And yet, we call it ‘relaxing.’ The tragedy isn’t the overdose - it’s that we’ve forgotten how to sit with discomfort without chemically erasing it.
i get what ur saying but sometimes you just need to unwind after a 12 hour shift and your back is killing you. i dont drink every day but when i do its one beer with my meds and i dont feel any different. maybe its just me but i think people need to stop acting like every combo is a death sentence
Of course they’re warning you about alcohol and opioids - but did you notice they didn’t mention the real culprit? The pharmaceutical industry funds these ‘awareness’ campaigns to make you think it’s your fault for mixing drugs, when they’re the ones pushing the prescriptions in the first place. OxyContin was marketed as non-addictive. Xanax was pushed as ‘safe for daily use.’ Now they’re blaming you for listening to the very people who sold you the poison. Wake up. This is a profit-driven slaughter.
yo i used to do speedballs back in college and let me tell u - it felt like flying and crashing at the same time. the first time i did it i thought i was gonna die. the second time i thought i was Jesus. third time? i ended up in the ER with my heart doing the cha-cha. no regrets? nah. but i also don’t think people who do this are monsters. they’re just trying to feel something real in a world that’s been numb since birth.
Thank you for this comprehensive and clinically accurate overview. It is imperative that public discourse on polypharmacy be grounded in evidence-based medicine rather than anecdotal experience or emotional rhetoric. I urge all readers to consult their prescribing physician before modifying any medication regimen, and to utilize verified pharmacological interaction databases such as Lexicomp or Micromedex for real-time risk assessment. Safety is not a suggestion - it is a responsibility.
I’ve sat with people who overdosed. I’ve held their hands while they were unconscious. I’ve watched families break apart because someone thought ‘just one’ wouldn’t hurt. But here’s the thing - the real problem isn’t the drugs. It’s the loneliness. The trauma. The lack of access to real care. If we treated addiction like a disease instead of a moral failure, we wouldn’t need these lists. We’d have therapy, housing, and community. Until then, yes - avoid the combos. But also ask why people feel like they need them in the first place.
you americans are so weak. in my country, we drink whiskey with painkillers since the 1980s and no one dies. you think everything is dangerous because you dont have real problems. go outside and see how people live. then come back and tell me about your little pills and wine. this post is for cowards.