Idiopathic Pulmonary Fibrosis (IPF): What You Need to Know
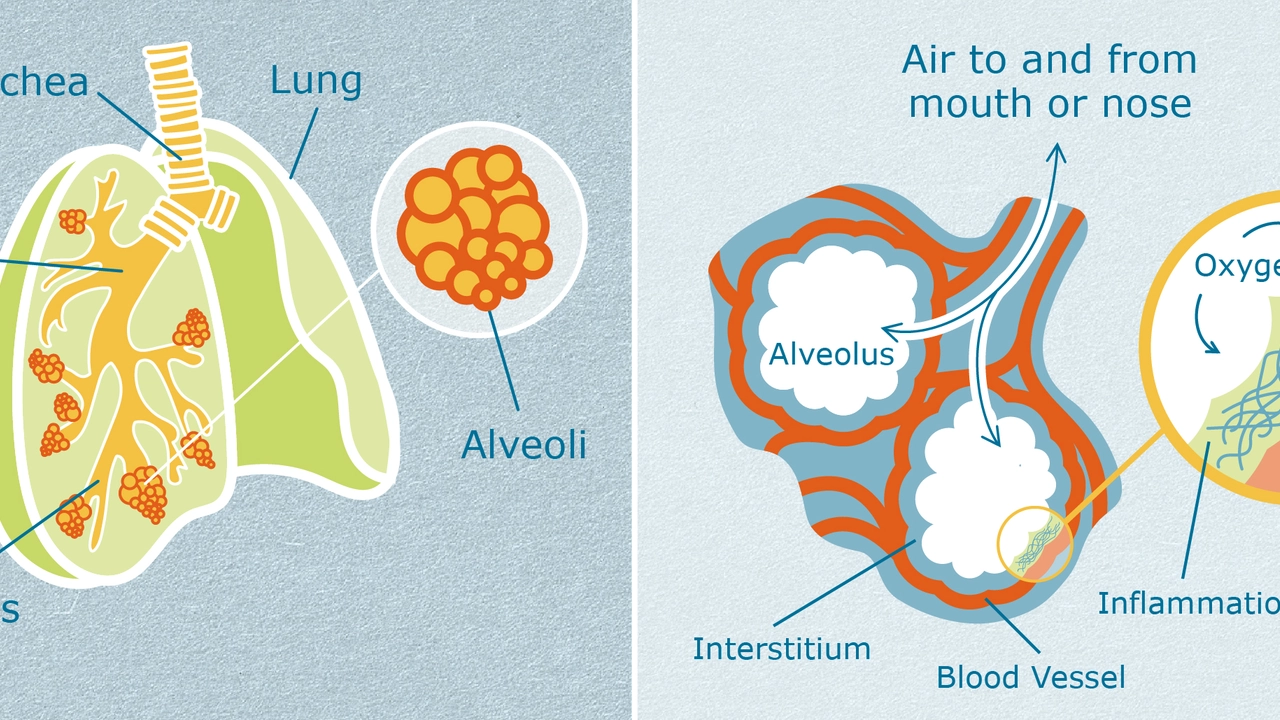
Idiopathic pulmonary fibrosis, or IPF, is a scary-sounding lung disease where scar tissue builds up in the lungs for no clear reason. That scar tissue makes the lungs stiff, so oxygen can’t get into the blood as easily. Over time, everyday activities like walking up stairs or even chatting can feel exhausting.
The word “idiopathic” simply means doctors don’t know the exact cause. Some researchers point to tiny inhaled particles, viral infections, or genetic factors, but no single trigger has been proven. Because the cause is unknown, the focus shifts to spotting the disease early and slowing its progress.
How IPF Shows Up
People with IPF usually notice a dry cough that won’t go away and a feeling of shortness of breath, especially during physical activity. The cough isn’t productive – you won’t cough up mucus – which often leads folks to ignore it at first. As the scar tissue spreads, even simple chores can leave you breathless.
Other signs include a subtle “crackling” sound when doctors listen to your lungs with a stethoscope, weight loss, and fatigue. These symptoms can look like other lung problems, so getting the right diagnosis matters.
Getting the Diagnosis Right
Doctors start with a medical history and a physical exam, then move on to imaging tests. A high‑resolution CT scan is the gold standard; it shows the pattern of scarring that points to IPF. Sometimes a lung biopsy is needed if the scan isn’t clear.
Blood tests help rule out other conditions, and pulmonary function tests measure how well your lungs are working. The combination of these tools gives a clear picture of whether IPF is the culprit.
Early diagnosis is key because treatments work best before the disease has advanced too far.
Treatment Options That Can Help
While there’s no cure for IPF, several medications can slow the scarring and improve quality of life. Two drugs approved by the FDA – pirfenidone and nintedanib – have shown to reduce the rate of decline in lung function. They’re taken daily and require regular monitoring for side effects like nausea or liver issues.
In addition to meds, lifestyle tweaks matter. Quitting smoking (if you smoke) is the single most important step. Pulmonary rehabilitation programs teach breathing exercises and gradual activity plans that help you stay active without overexerting yourself.
Oxygen therapy becomes necessary when blood oxygen levels drop. Modern portable oxygen devices let you move around more freely, and many patients report feeling less tired once they start using supplemental oxygen.
For a small group of patients with severe disease, a lung transplant can be life‑changing. Transplant teams evaluate candidates carefully, considering age, overall health, and how quickly the disease is progressing.
Living with IPF: Practical Tips
Stay on top of appointments. Regular follow‑ups let your doctor adjust treatment before problems get worse. Keep a symptom diary – note when you feel short of breath, how long you can walk, and any new cough patterns. This record helps your doctor see trends and act fast.
Plan your day with rest breaks. If you notice you get winded after a few minutes of walking, pause, breathe, then continue. Over time, you’ll find a rhythm that keeps you comfortable.
Connect with support groups, either online or in your community. Hearing how others manage IPF can offer new coping ideas and emotional relief.
Finally, stay informed. New research on antifibrotic drugs and stem‑cell therapy is always emerging. Ask your healthcare team about clinical trials that might be a fit for you.
Idiopathic pulmonary fibrosis is a tough diagnosis, but with early detection, appropriate medication, and lifestyle adjustments, many people keep leading active, fulfilling lives. Keep asking questions, track your health, and work closely with your care team – that’s the best strategy for living well with IPF.