Oxygen Therapy: What It Is, When It Helps, and How to Use It Safely
Ever wondered why doctors hand out small oxygen tanks or set up humming machines at night? It’s not a sci‑fi gimmick – supplemental oxygen is a real, proven tool for people who can’t get enough air on their own. Whether you have COPD, a heart condition, or get short‑of‑breath after a cold, oxygen therapy can make everyday tasks feel easier.
Why Doctors Recommend Oxygen Therapy
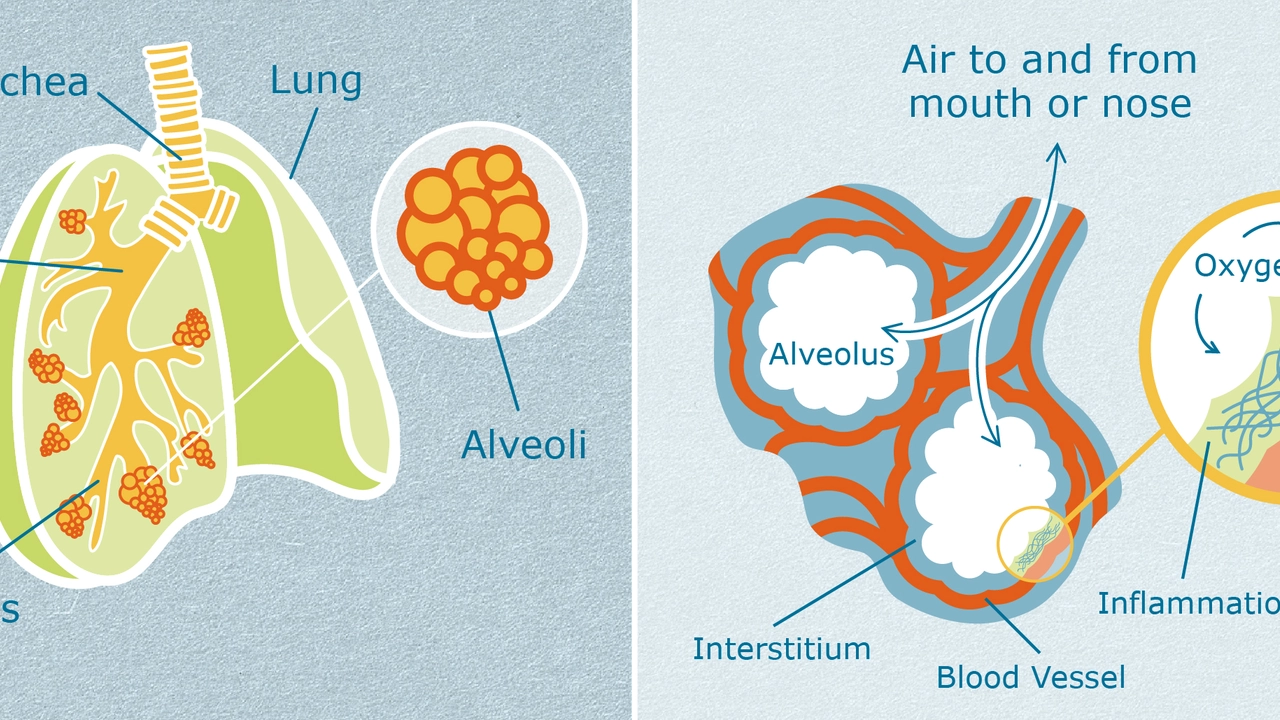
Doctors prescribe oxygen when blood‑oxygen levels drop below a healthy range (usually under 90%). Low oxygen can cause fatigue, headaches, and even worsen heart problems. By delivering extra oxygen, the body’s cells get the fuel they need, which reduces strain on the heart and improves energy levels. Most patients notice better sleep, less breathlessness during walks, and a faster recovery after surgery.
Getting Started at Home or in a Clinic
If your doctor says you need supplemental oxygen, the first step is a proper assessment. A simple pulse‑oximeter test measures how much oxygen is in your blood while you rest and while you move. Based on those numbers, a respiratory therapist will suggest a flow rate – usually measured in liters per minute (LPM). Home setups often include a small concentrator that pulls oxygen from the air, while clinics might use larger tanks for short‑term use.
Setting up a home system is easier than it sounds. The concentrator sits on a flat surface near an outlet, and a lightweight nasal cannula delivers the gas right into your nostrils. Most people find the cannula comfortable after a day or two. If you need a mask for higher flow rates, the therapist will show you how to fit it snugly without feeling claustrophobic. Remember to keep the equipment clean and check the tubing for cracks regularly – a leak can waste oxygen and lower the therapy’s effectiveness.
Safety matters. Never smoke near oxygen equipment, as the gas makes flames burn hotter. Store tanks upright and out of direct sunlight. If you travel, ask your pharmacy about portable concentrators or small cylinders that meet airline regulations. Knowing these basics keeps you safe and ensures you get the full benefit of each breath.
While oxygen can feel like a magic fix, it’s not a cure‑all. It works best when combined with other healthy habits: quit smoking, stay active, and follow any medication plan your doctor gave you. If you notice skin irritation from the cannula, try a softer size or a cloth barrier. If you feel dizzy, light‑headed, or notice a sudden drop in oxygen saturation, call your doctor right away – you may need a dosage adjustment.
What about the cost? Many insurance plans cover durable medical equipment, including concentrators, if you have a prescription. Check with your provider to avoid surprise bills. Some pharmacies also offer rental programs, which can be cheaper than buying a brand‑new unit.
In a nutshell, oxygen therapy is a practical way to boost your body’s oxygen supply when you can’t get enough on your own. It improves energy, sleep, and overall quality of life for millions of people. By following a clear prescription, keeping your equipment clean, and staying mindful of safety rules, you’ll get the most out of every breath.
Hi there! Today's post is about exploring the role of oxygen therapy in managing a respiratory condition called Idiopathic Pulmonary Fibrosis. We'll delve into how this treatment method can optimize the quality of life for those living with this disease. It's a fascinating insight into a topic that seldom gets the attention it deserves but is so critical to millions of people. Join me as we delve into this important aspect of pulmonary health care.
Read More