Torsades de Pointes from QT-Prolonging Medications: How to Recognize and Prevent This Life-Threatening Reaction

QT-Prolonging Medication Risk Checker
Medication Risk Assessment Tool
Enter medications you're taking to check for QT-prolonging risk and Torsades de Pointes danger. This tool helps identify high-risk medications based on CredibleMeds database guidelines.
Torsades de Pointes isn’t just another arrhythmia. It’s a sudden, chaotic heart rhythm that can kill in minutes - and it’s often triggered by medications you or someone you know might be taking right now. Unlike a heart attack, there’s usually no chest pain. No warning. Just a fainting spell, or worse - sudden cardiac arrest. The good news? It’s almost always preventable if you know what to look for.
What Exactly Is Torsades de Pointes?
Torsades de Pointes (TdP) is a rare but deadly type of ventricular tachycardia. On an ECG, it looks like the QRS complexes are twisting around the baseline - hence the name, which means "twisting of the points." It doesn’t happen out of nowhere. It only occurs when the heart’s electrical recovery phase - measured as the QT interval - is abnormally long.The QT interval shows how long it takes the heart’s lower chambers to recharge between beats. When this interval stretches too long, the heart muscle cells don’t reset properly. That’s when abnormal electrical sparks, called early afterdepolarizations, can trigger TdP. It’s not a slow, gradual decline. It’s an electrical short-circuit that can spiral into ventricular fibrillation and death within seconds.
Most cases are drug-induced. Over 200 medications - from antibiotics to antidepressants - can interfere with the hERG potassium channel, which controls the heart’s repolarization. Block that channel, and you delay the heart’s reset. The longer the delay, the higher the risk.
Which Medications Are the Biggest Culprits?
Not all QT-prolonging drugs carry the same risk. Some are high-risk, others are conditional. The CredibleMeds database classifies them into three tiers:- Known Risk: Clear evidence of TdP. Includes sotalol, dofetilide, quinidine, haloperidol, thioridazine, ziprasidone, citalopram (over 40 mg/day), escitalopram (over 20 mg/day), methadone (especially above 100 mg/day), ondansetron (over 16 mg IV), and ketoconazole.
- Possible Risk: Theoretical or limited data. Includes azithromycin, moxifloxacin, domperidone (now downgraded from "Known" in 2023), and fluoxetine.
- Conditional Risk: Only dangerous if combined with other factors like low potassium or liver disease. Includes some antifungals and antidepressants.
What’s surprising? Many of these aren’t heart drugs. They’re common prescriptions: antibiotics for sinus infections, antidepressants for anxiety, anti-nausea meds for chemo, and even methadone for chronic pain. The FDA has issued black box warnings for 37 of them. Terfenadine (Seldane) and cisapride (Propulsid) were pulled off the market entirely because of TdP deaths.
Who’s Most at Risk?
It’s not just about the drug. It’s about the person taking it. About 70% of TdP cases happen in women. Over two-thirds of cases occur in people over 65. And nearly half of those affected already have heart disease.The biggest modifiable risk factors? Electrolytes.
- Hypokalemia (low potassium): Present in 43% of cases. When potassium drops below 3.5 mmol/L, TdP risk jumps 3.2 times.
- Hypomagnesemia (low magnesium): Found in 31% of cases. Magnesium below 1.6 mg/dL raises risk by 2.7 times.
- Bradycardia: Heart rate under 60 bpm increases risk - slower heart rate means longer time between beats, giving more room for abnormal rhythms to form.
- Drug interactions: Taking two QT-prolonging drugs together raises risk by 63%. Combining clarithromycin with citalopram, for example, can be dangerous.
- Renal or liver impairment: Citalopram TdP cases increased 4.8-fold in patients with severe kidney disease because the drug builds up.
People with inherited long QT syndrome - like Romano-Ward (1 in 2,000) or Jervell and Lange-Nielsen (1 in 1 million) - are at extreme risk. But most TdP cases happen in people who didn’t know they had a genetic predisposition.
How Do You Spot It Before It’s Too Late?
You can’t feel TdP coming. But you can catch it on an ECG - if you’re looking.The red flags:
- QTc interval > 500 ms - this doubles or triples your risk.
- QTc increase of 60 ms or more from baseline - even if it’s still under 500 ms.
- Prominent U waves - small waves after the T wave, a classic sign of delayed repolarization.
- Labile QT - QT interval that changes dramatically from beat to beat.
- "Short-long" cycle pattern - a short heartbeat followed by a long pause, then TdP kicks in.
Baseline ECGs are critical. Before starting high-risk meds like methadone, citalopram, or ondansetron, get an ECG. Repeat it after a few days or when the dose is increased. Don’t assume normal baseline means safe - electrolyte shifts can turn a safe drug into a deadly one.
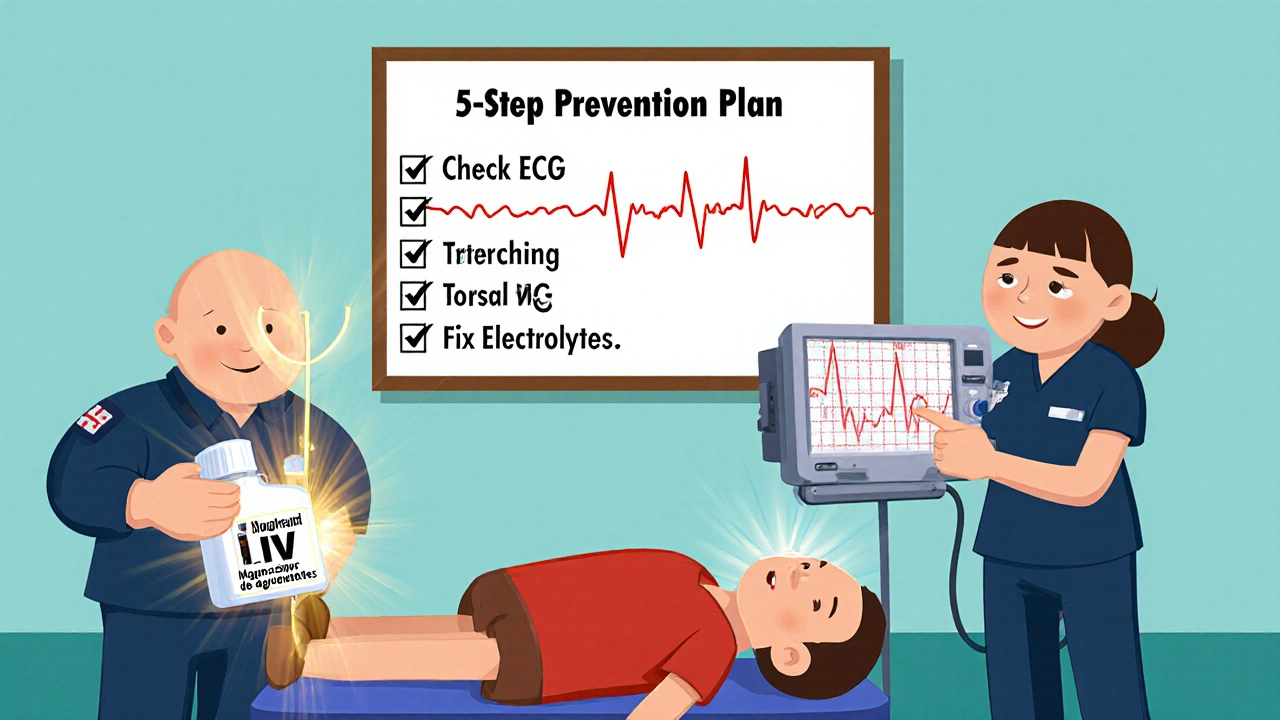
How to Prevent It - A Practical 5-Step Plan
Prevention isn’t complicated. It’s systematic.- Screen for inherited LQTS. Use the Schwartz score: family history, unexplained fainting, ECG findings. If score ≥3.5, avoid QT-prolonging drugs entirely.
- Check electrolytes. Get potassium and magnesium levels before and during treatment. Keep potassium above 4.0 mmol/L and magnesium above 2.0 mg/dL.
- Review all meds. Use CredibleMeds.org to check every drug - including OTC and supplements. Even some antacids and herbal products can interact.
- Get a baseline ECG. Especially if you’re over 65, female, or on multiple meds. Measure QTc using Bazett’s formula: QTc = QT / √RR.
- Set up monitoring. For methadone >100 mg/day: repeat ECG at 1 week and then monthly. For citalopram: cap at 20 mg/day if over 60. For ondansetron: avoid IV doses over 16 mg.
VA Healthcare data from 2018-2022 showed that following these steps reduced TdP cases by 78%.
What If TdP Happens? Emergency Response
If someone collapses with suspected TdP, time is everything.Immediate actions:
- Give magnesium sulfate: 1-2 grams IV over 5-15 minutes. Works in 82% of cases - even if magnesium levels are normal.
- Correct electrolytes: Potassium and magnesium IV if levels are low.
- Pace the heart: Temporary transcutaneous pacing to keep heart rate above 90 bpm. This shortens the QT interval and stops the arrhythmia. Works in 76% of cases.
- Isoproterenol: If pacing isn’t available, this drug increases heart rate and suppresses abnormal rhythms. Use with caution - it can worsen other arrhythmias.
- Defibrillate if needed: If TdP turns into ventricular fibrillation, shock immediately.
Never give drugs that prolong QT further - like amiodarone or sotalol. They’ll make it worse.
The Bigger Picture: Regulation, Costs, and New Tools
Since 2005, every new drug must pass a thorough QT study under ICH E14 guidelines. That adds over $1 million and 8 months to development. The global QT testing market hit $412 million in 2022.The FDA now encourages risk-based decisions, not blanket bans. A drug with a small QT effect might still be worth it if it saves lives - as long as you monitor.
New tools are emerging. Mayo Clinic’s machine learning model predicts individual TdP risk with 89% accuracy by analyzing 17 variables - age, gender, kidney function, drug combo, baseline QTc. The TENTACLE registry is refining risk thresholds: QTc >520 ms with a delta >70 ms from baseline now predicts TdP with 94% accuracy.
And the PREVENT TdP Act, proposed in 2022, could standardize ECG monitoring nationwide. If passed, it could prevent 200+ deaths a year - at a cost of $227 million annually. The math is clear: prevention is cheaper than death.

9 Comments
lol so now i gotta get an ekg before taking my zpack? 🤡 my doc just wrote it and i'm fine. everyone's paranoid these days. next they'll make us check our qr codes before breathing.
this is actually super helpful. i work in a clinic and we've had a few close calls with meds like citalopram and azithromycin. just remembering to check potassium and do a baseline ekg saves lives. thanks for laying it out so clear 😊
i'm curious - how often do people actually get baseline ekg's before starting methadone or citalopram? i feel like in real practice, especially in primary care, it's more of a suggestion than a standard. is there data on compliance?
The claim that '70% of TdP cases happen in women' is misleading without context. Women have longer baseline QT intervals due to hormonal differences - this is physiological, not pathological. The real issue is undermonitoring in elderly female patients on polypharmacy, not gender itself. Also, 'QTc >500ms doubles risk' is outdated - recent studies show the curve is nonlinear and steepens after 550ms. CredibleMeds needs updating.
It is imperative to underscore, with the utmost gravity, that the prevention of Torsades de Pointes is not merely a clinical recommendation - it is a moral obligation incumbent upon every prescriber, pharmacist, and healthcare system. The integration of systematic ECG screening, electrolyte monitoring, and comprehensive medication reconciliation constitutes the very foundation of patient safety in modern pharmacotherapy. Failure to implement these measures, particularly in vulnerable populations such as the elderly, the female demographic, and those with renal impairment, constitutes not negligence, but a systemic dereliction of duty. The VA data demonstrating a 78% reduction in incidence is not merely encouraging - it is a clarion call for universal adoption of these protocols across all care settings, regardless of resource constraints.
this is why i hate modern medicine. they turn every little thing into a death sentence. i took azithromycin last year and lived. now i'm supposed to get an ekg? and check magnesium? who even has time for this? they're just trying to scare us so we pay for more tests. #medicalindustryscam
I cannot emphasize enough how critical this information is. Every clinician - from ER physicians to primary care providers - must internalize these five steps. The fact that preventable deaths are still occurring is unacceptable. We must advocate for institutional protocols: mandatory baseline ECGs for all patients over 50 on QT-prolonging agents, automated alerts in EHRs when high-risk combinations are prescribed, and mandatory electrolyte checks before IV ondansetron. This isn't optional. It's standard of care.
i just keep thinking about how we're all just tiny sparks in this big electrical machine called the body. one little delay in the reset… and boom. it’s wild how something so simple - like a low potassium level - can flip the switch on something that kills. we’re so quick to pop pills but forget we’re holding live wires. maybe we need to slow down. not just the meds… but us. breathe. check the numbers. be gentle with the body. it’s trying to work with what we give it.
mg >2.0 and k >4.0. got it. thanks.