Tricyclic Antidepressants and Antihistamines: Avoiding Anticholinergic Overload

Anticholinergic Cognitive Burden Calculator
How to Use
Enter your medications to calculate the cumulative anticholinergic burden (ACB) score. This score helps you understand your risk of cognitive decline and anticholinergic side effects.
- Enter a medication name or select from the dropdown
- Click 'Add to List' to include it in your calculation
- See your total ACB score and risk level
- Click 'Clear' to reset the calculator
Your Medications
Your Cumulative ACB Score
Total ACB Score:
This score indicates your anticholinergic burden risk level
Score: 0-2 = Low Risk
Score: 3 = Moderate Risk
Score: 4+ = High Risk
What Your Score Means
Enter your medications to see your ACB score and what it means.
Recommended Actions:
- For low risk (0-2): Continue monitoring but no immediate changes needed
- For moderate risk (3): Discuss alternatives with your doctor
- For high risk (4+): Consider discontinuing or replacing high-burden medications
Combining tricyclic antidepressants (TCAs) with first-generation antihistamines like diphenhydramine (Benadryl) isn’t just a mild interaction-it’s a silent risk that can land someone in the ER. This isn’t theoretical. In 2020, a study of over 3,300 patients found more than 6,800 high-risk alerts triggered when these drugs were prescribed together. And it’s happening more often than you think, especially in older adults who are already on multiple medications.
How Anticholinergic Overload Works
Your body uses acetylcholine to control everything from memory and focus to digestion and bladder function. When drugs block this chemical, they cause anticholinergic effects. Tricyclic antidepressants like amitriptyline and imipramine were designed to affect serotonin and norepinephrine, but they also strongly block muscarinic receptors-the same receptors targeted by antihistamines like diphenhydramine. When taken together, their effects add up. This isn’t 1 + 1 = 2. It’s more like 1 + 1 = 4.The result? A buildup of anticholinergic burden. Think of it like filling a cup with water. One drug fills it halfway. The other pours in another half. Now the cup overflows. That overflow is what doctors call anticholinergic overload. Symptoms include confusion, dry mouth, blurred vision, constipation, urinary retention, rapid heartbeat, and memory lapses. In older adults, it can look like dementia-or even trigger acute delirium.
Who’s at Risk?
People over 65 are the most vulnerable. Their livers and kidneys don’t clear drugs as quickly. Their brains are more sensitive to acetylcholine disruption. But it’s not just age. Anyone taking multiple medications that have anticholinergic properties is at risk. A 2021 survey found that 37% of pharmacists see at least one case of anticholinergic overload every month. And nearly 3 out of 10 of those cases involve TCAs mixed with antihistamines.Even healthy-looking patients can be affected. A Reddit user, a medical resident, shared that they’d seen three elderly patients admitted for delirium-all had been prescribed diphenhydramine for sleep while already on amitriptyline for pain or depression. Their doctors didn’t realize the combination was dangerous. One patient ended up in the ER with urinary retention and severe confusion. The diagnosis? Anticholinergic toxicity.
Why This Isn’t Going Away
You might think TCAs are outdated. They’re not. For neuropathic pain, fibromyalgia, and some types of chronic depression, they’re still first-line. Amitriptyline, in particular, is widely prescribed for nerve pain because it works better than SSRIs for many patients. Meanwhile, diphenhydramine is still the go-to sleep aid for millions. It’s cheap. It’s available over the counter. And many people don’t think of it as a real drug.But here’s the problem: diphenhydramine has an Anticholinergic Cognitive Burden (ACB) score of 2. Amitriptyline scores a 3-the highest possible. Together, that’s a total of 5. Research shows that a cumulative ACB score of 3 or higher doubles the risk of dementia over time. A 2015 JAMA study found that people taking medications with high anticholinergic burden had a 54% higher chance of developing dementia over 10 years.
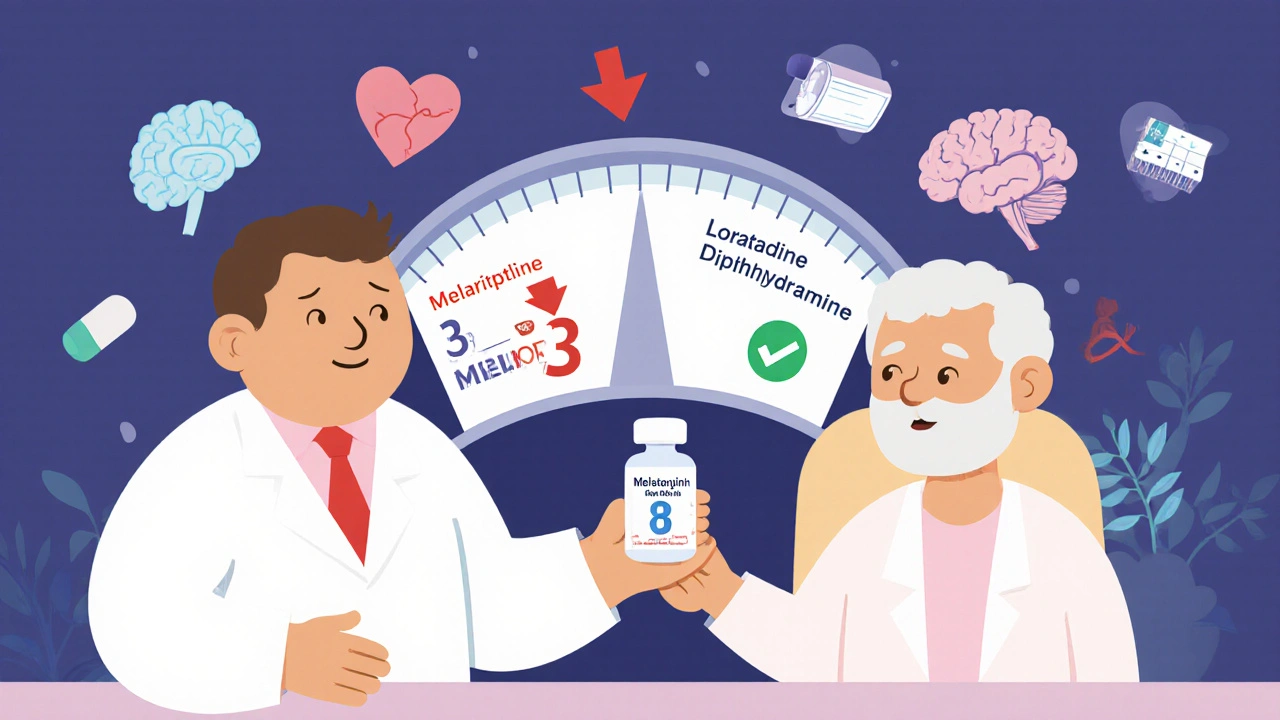
What’s Safer?
Not all antihistamines are the same. Second-generation options like loratadine (Claritin), cetirizine (Zyrtec), and fexofenadine (Allegra) barely touch acetylcholine receptors. Their ACB score is 0. If you need an antihistamine for allergies or sleep, these are the clear alternatives.For sleep, melatonin (0.5-5 mg) is a safer, non-anticholinergic option. It doesn’t cause grogginess, memory issues, or urinary problems. It also doesn’t interact with TCAs. Many patients report better sleep quality on melatonin than on diphenhydramine-without the side effects.
As for antidepressants, not all TCAs are equal. Nortriptyline and desipramine have lower anticholinergic effects than amitriptyline or clomipramine. If you’re on a TCA and need to reduce risk, talk to your doctor about switching to one of these. And if you’re on an SSRI like sertraline or fluoxetine, avoid combining it with a TCA-those combinations carry their own risks, including serotonin syndrome.
What Doctors Are Doing About It
Awareness is rising. In 2018, only 32% of psychiatrists routinely checked for cumulative anticholinergic burden. By 2023, that number jumped to 78%. Electronic health records like Epic now block prescriptions for TCA-antihistamine combos. If a doctor tries to write both, the system pops up a hard stop with a warning.The American Geriatrics Society’s Beers Criteria (2023 update) explicitly says: avoid first-generation antihistamines in older adults taking TCAs. The FDA now requires updated labeling on all TCAs and diphenhydramine products to warn about cumulative anticholinergic effects.
And it’s working. The American Geriatrics Society’s ‘Anticholinergic Burden Audit’ found that 41% of inappropriate TCA-antihistamine combinations were stopped in participating clinics within six months. Patients who had these drugs deprescribed saw a 34% reduction in cognitive decline over 18 months.

What You Should Do
If you’re taking a TCA like amitriptyline, clomipramine, or imipramine:- Check every medication you take-even OTC ones-for anticholinergic effects.
- Replace diphenhydramine (Benadryl), hydroxyzine, or promethazine with loratadine, cetirizine, or melatonin.
- Ask your doctor to calculate your total ACB score. You can do this yourself using the Anticholinergic Cognitive Burden scale-amitriptyline = 3, diphenhydramine = 2, fexofenadine = 0.
- Get your cognitive function checked annually with a simple test like the MMSE. A score below 24 could signal anticholinergic toxicity.
- If you’ve had unexplained confusion, memory lapses, or trouble urinating since starting a new med, bring this up immediately.
Don’t assume your doctor knows. A 2022 study found that 60% of primary care providers didn’t recognize the cumulative risk of TCA-antihistamine combinations. Be your own advocate. Write down every pill you take-prescription, supplement, OTC-and bring it to your next appointment.
It’s Not Just About Sleep
Many people think diphenhydramine is harmless because it’s sold as a sleep aid or allergy pill. But it’s not a vitamin. It’s a potent anticholinergic. And when paired with a TCA, it becomes a hidden danger. The same goes for other common OTC drugs like dimenhydrinate (Dramamine) or oxybutynin (for overactive bladder)-all carry anticholinergic risk.The truth? You don’t need to suffer through poor sleep or allergies to protect your brain. Safer alternatives exist. And avoiding this combination isn’t about giving up treatment-it’s about choosing better ones.
Can I take Benadryl with amitriptyline?
No. Combining diphenhydramine (Benadryl) with amitriptyline significantly increases the risk of anticholinergic overload. This can lead to confusion, urinary retention, rapid heartbeat, and even delirium, especially in older adults. Both drugs block acetylcholine, and together they overwhelm the system. Switch to a second-generation antihistamine like loratadine or a non-anticholinergic sleep aid like melatonin instead.
What are the signs of anticholinergic overload?
Symptoms include dry mouth, blurred vision, constipation, trouble urinating, fast heartbeat, confusion, memory problems, hallucinations, and extreme drowsiness. In older adults, these often look like dementia or a sudden mental decline. If you or a loved one starts showing these symptoms after starting a new medication, stop the drug and seek medical help immediately.
Are all antidepressants risky with antihistamines?
No. Only tricyclic antidepressants (TCAs) like amitriptyline, imipramine, and clomipramine have strong anticholinergic effects. SSRIs like sertraline or fluoxetine and SNRIs like venlafaxine have much lower risk. However, combining TCAs with SSRIs can still cause serotonin syndrome. Always check drug interactions before mixing any antidepressant with antihistamines.
Is there a test to measure anticholinergic burden?
Yes. The Anticholinergic Cognitive Burden (ACB) scale assigns points to medications based on their anticholinergic strength. Amitriptyline = 3, diphenhydramine = 2, loratadine = 0. Add up the scores of all your meds. A total of 3 or higher increases dementia risk. Many pharmacies and electronic health systems now use this scale to flag risky combinations.
Why are TCAs still used if they’re so risky?
TCAs are still first-line for certain conditions like neuropathic pain, fibromyalgia, and some treatment-resistant depressions because they work better than SSRIs for these issues. The key is using them carefully-choosing lower-risk TCAs like nortriptyline, avoiding anticholinergic add-ons, and monitoring for side effects. For many, the benefits outweigh the risks when managed properly.
Can anticholinergic damage be reversed?
In many cases, yes. Stopping high-burden medications can lead to noticeable improvement in cognition and function within weeks. A 2023 study showed that elderly patients who had anticholinergic drugs discontinued saw a 34% reduction in cognitive decline over 18 months. The earlier you act, the better the outcome.

13 Comments
man i had no idea benadryl was such a sneaky little monster when mixed with amitriptyline 😅 i’ve been taking it for years for sleep and honestly thought it was just a sleepy pill like tylenol pm. my grandma got super confused last winter and the doc said it was ‘just aging’ but now i think it was this combo. gonna check her meds tonight. thanks for the wake up call
so many people dont realize otc meds can be just as dangerous as prescriptions i used to give my dad diphenhydramine for his allergies and he was on nortriptyline for nerve pain and he kept forgetting where he put his keys and saying weird things i thought he was just getting old until i read this now hes on cetirizine and hes like a new person
This is a profoundly important post from a public health perspective. In India, we see similar patterns where elderly patients are prescribed multiple anticholinergic agents without awareness of cumulative burden. The cultural normalization of 'sleeping pills' and 'allergy tablets' as harmless is dangerous. I have seen patients in rural clinics on amitriptyline with promethazine for nausea and diphenhydramine for insomnia - total ACB score of 8. It is not hyperbole to say this is a silent epidemic. Education must reach primary care and pharmacy levels.
you know… i used to think doctors knew everything. i trusted them. then my uncle went into delirium after being on amitriptyline and benadryl for months. he didn’t even know he was taking both. the pharmacist didn’t say anything. the doctor didn’t ask. it took a family member to read the labels. i’m not angry anymore. i’m just… sad. and careful.
just wanted to say i switched from diphenhydramine to melatonin after reading this and honestly my sleep is better now? no more morning fog, no dry mouth, and i don’t feel like i’m walking through peanut butter all day. also my wife says i’m less grumpy in the morning which is a win. i didn’t even know how bad the side effects were until i stopped them. melatonin’s not magic but it’s way less scary than a brain fog grenade
my mom took benadryl for years and started having trouble peeing and got super confused once at the grocery store they thought she had alzheimers but it was just the combo with her tricyclic she got switched to zyrtec and boom like night and day i wish more people knew this
we live in a world where we treat chemicals like candy and then act shocked when our brains start glitching. diphenhydramine isn’t a sleep aid it’s a chemical restraint. and amitriptyline? it’s not just an antidepressant it’s a neurochemical sledgehammer. when you stack them? you’re not treating symptoms you’re erasing yourself slowly. and nobody talks about it because it’s not sexy. it’s not a viral trend. it’s just… people forgetting their grandkids’ names because the system didn’t care enough to warn them
ACB score of 5. High risk. Avoid. Period.
omg this is so important!! 🙏 i just told my aunt to ditch her benadryl and try melatonin and she said ‘but it’s just a pill’ and i was like ‘but it’s a brain-slowing pill’ 😅 she’s on amitriptyline too and now she’s reading this and crying because she didn’t know. thank you for posting!! 🤍
if you’re on a TCA and using OTC sleep aids, you’re playing russian roulette with your cognition. don’t wait for delirium to hit. audit your meds now. write them down. look up each one’s ACB score. swap out the 2s and 3s for 0s. your future self will thank you. this isn’t fearmongering - it’s harm reduction.
it’s not just about drugs - it’s about our society’s pathological disregard for the aging brain. we medicate away symptoms instead of asking why the body is signaling distress. diphenhydramine isn’t the villain - it’s the symptom of a system that values convenience over consciousness. we’ve turned sleep into a problem to be pharmacologically erased, and cognition into an afterthought. this post? it’s not a warning. it’s a eulogy for the quiet dementia we’re all being slowly drugged into.
the ACB scale is underutilized in clinical practice despite robust validation. the 2015 JAMA study and subsequent meta-analyses show dose-dependent dementia risk. EHR integration has improved, but provider education lags. Pharmacists are critical gatekeepers here - yet many lack formal training in cognitive burden metrics. Standardizing ACB scoring in med reconciliation protocols could prevent thousands of iatrogenic events annually.
in my village in Uttar Pradesh, grandfathers take diphenhydramine for colds and amitriptyline for back pain. no one checks. no one asks. the pharmacy sells both. the doctor prescribes both. they say ‘it’s just medicine’. I showed them this post. One man stopped his benadryl. He remembered his wife’s name again after three months. That’s not science. That’s a miracle.