Medical Weight Management: Clinics, Medications, and Monitoring

When you hear the word obesity, what comes to mind? Maybe diet pills, gym memberships, or a well-meaning friend saying, "Just eat less and move more." But if you’ve tried that and it didn’t stick, you’re not alone. And you’re not failing-you’re just dealing with a chronic disease that’s been misunderstood for decades.
Today, medical weight management isn’t about willpower. It’s about science. It’s about teams of doctors, dietitians, and behavioral coaches working together to treat obesity like diabetes or high blood pressure: with ongoing care, proven medications, and real monitoring. The American College of Cardiology’s 2025 guidelines made it official: obesity is a chronic disease, and it deserves the same level of clinical attention as any other.
What Medical Weight Management Actually Looks Like
Medical weight management isn’t a program you sign up for online. It’s a structured, multidisciplinary approach that starts with a clear diagnosis. To qualify, you typically need a BMI of 30 or higher-or a BMI of 27 or higher if you have conditions like type 2 diabetes, high blood pressure, or sleep apnea. That’s not arbitrary. These thresholds are based on decades of data showing when health risks start rising significantly.
Once you’re in, the process begins with orientation. Many clinics, like West Virginia University Health System’s program, require patients to watch a pre-recorded session and read a detailed handbook before their first appointment. Why? Because this isn’t a quick fix. You need to understand what you’re getting into: regular check-ins, tracking your food and activity, and learning how to manage triggers that lead to eating when you’re not hungry.
Then comes the team. A physician oversees your care. A registered dietitian creates a personalized meal plan-not a one-size-fits-all diet, but a plan built around your food preferences, cultural habits, and schedule. A behavioral health specialist helps you identify emotional eating patterns, stress triggers, and sleep issues that sabotage progress. This isn’t optional. Studies show that programs with all three components achieve nearly double the weight loss of those without.
The Medications: Beyond Willpower
Medication is now a core part of treatment-not a last resort. The two most effective drugs approved for long-term use are semaglutide (Wegovy®) and tirzepatide (Zepbound®). Both are GLP-1 receptor agonists, originally developed for type 2 diabetes, but their impact on weight is staggering.
In clinical trials, semaglutide led to an average weight loss of 14.9% after 72 weeks. Tirzepatide? 20.2%. That’s not a few pounds. That’s a 50-pound loss for someone who weighs 250. And it’s not just about the scale. These drugs reduce liver fat, improve insulin sensitivity, lower blood pressure, and decrease the risk of heart attack and stroke-especially in people with diabetes.
There’s a new contender: retatrutide, a triple agonist that targets GLP-1, GIP, and glucagon receptors. Early phase 2 trials showed 24.2% average weight loss in just 48 weeks. It’s not FDA-approved yet, but it’s coming fast.
Still, access is a huge problem. Only 68% of commercial insurance plans cover these medications in 2025. Medicare Advantage plans cover them in just 12% of cases. For many, the monthly cost can be $1,000 or more without insurance. Some clinics offer payment plans or work with patient assistance programs, but the gap between need and access remains wide.
Monitoring: It’s Not Just About the Scale
Weight loss isn’t linear. You’ll have weeks where the scale doesn’t budge. That’s normal. But in a medical program, you’re not left guessing why.
At every visit, your team checks more than your weight. They measure waist circumference, track blood pressure, review lab results (like fasting glucose and liver enzymes), and ask about sleep, stress, and mood. These are the real markers of health improvement.
The American Diabetes Association’s 2025 guidelines recommend monitoring at least every three months during active treatment. Some clinics use digital tools-like the MyWVUChart app-to let patients log meals, activity, and moods between visits. One patient on Reddit said this feature helped her realize she was eating more on weekends because she felt guilty about skipping workouts. That kind of insight? That’s what changes outcomes.
And it works. A 2024 JAMA Internal Medicine study found that people in medically supervised programs lost 9.2% of their body weight in a year. In commercial programs? Just 5.1%. The difference? Professional oversight, medication access, and consistent monitoring.
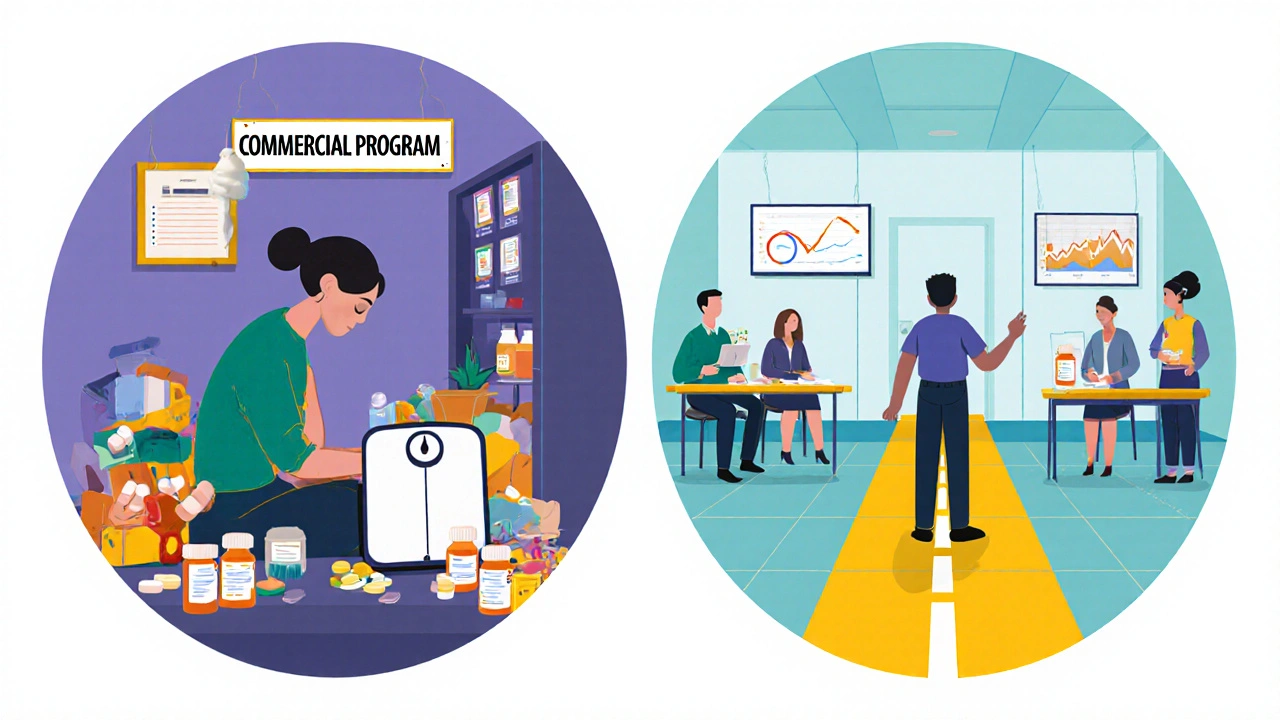
Clinics vs. Commercial Programs: The Real Difference
There are thousands of weight loss programs out there: meal delivery services, apps with coaches, online communities. Some are helpful. But they’re not medical.
Medical clinics are staffed by licensed professionals who can diagnose underlying conditions, adjust medications, and respond to complications. They use electronic health records to track your progress over time and coordinate with your primary care doctor. They follow evidence-based guidelines-not trends.
Cost-wise, medical programs run $150-$300 a month. Commercial programs? $20-$60. But here’s the catch: commercial programs rarely deliver lasting results. One study showed 80% of people who lost weight in a commercial program regained it within two years. In medical programs, 70% maintain at least 5% weight loss after one year.
And then there’s the environment. A 2025 survey by the Obesity Action Coalition found that 58% of patients praised the “non-judgmental” atmosphere in medical clinics. Contrast that with online forums where people are told they’re “lazy” or “lack discipline.” Medical weight management treats you as a patient-not a problem to be solved.
Who’s Getting Left Behind
Despite all the progress, disparities are glaring. Black and Hispanic patients are 43% less likely to be offered weight-loss medications-even when they meet the same BMI and health criteria as white patients. That’s not a gap in access. That’s a gap in care.
Language barriers, provider bias, and lack of culturally tailored resources play a role. Some clinics are starting to fix this: hiring multilingual staff, offering materials in Spanish and other languages, and training providers to recognize their own unconscious biases. The ACC’s 2025 guidelines even include specific recommendations: use chairs without armrests, provide blood pressure cuffs in multiple sizes, and never say, “You just need to try harder.”
Employers are stepping in too. Nearly half of Fortune 500 companies now offer medical weight management as part of their health benefits. That’s up from 18% in 2022. For many employees, this is the only way they can afford treatment.
What Success Really Looks Like
Success isn’t hitting a magic number on the scale. It’s being able to walk up stairs without getting winded. It’s getting off your blood pressure meds. It’s sleeping through the night. It’s feeling confident enough to go to a family gathering without dreading the comments.
One patient told her dietitian she stopped avoiding mirrors after losing 12% of her weight. Another said she started taking her kids to the park because she could finally keep up with them. These aren’t side effects. They’re the point.
And the data backs it up. Every $1 spent on medical weight management saves $2.87 in reduced healthcare costs for diabetes and heart disease within five years. That’s not just personal gain-it’s a public health win.
Obesity isn’t a moral failing. It’s a complex, biological condition. And the tools to treat it effectively are here. The question isn’t whether you can do it. It’s whether the system will let you.
Is medical weight management right for me?
Medical weight management is designed for people with obesity (BMI ≥30) or overweight with related health conditions (BMI ≥27). If you’ve tried dieting and exercise without lasting results, or if you have type 2 diabetes, high blood pressure, or sleep apnea, this approach is likely more effective than self-directed efforts. It’s especially helpful if you’re open to medication and regular follow-ups.
How long does medical weight management take?
It’s a long-term process. Most people see meaningful weight loss within 3-6 months, but the goal is sustained change. The American Diabetes Association recommends ongoing treatment for at least one year, with many patients continuing for several years. Like managing high blood pressure, stopping treatment often leads to weight regain. The focus is on lifelong health, not a short-term number.
Do I need to be on medication?
No, but it significantly improves outcomes. Medications like semaglutide and tirzepatide are not magic pills-they work best when combined with diet, movement, and behavior changes. But for many, they’re the missing piece. Without medication, losing 10% of body weight is rare. With it, that becomes achievable for most patients. Your provider will help you decide based on your health goals, insurance coverage, and personal preferences.
Can I get these medications from my regular doctor?
Some primary care doctors now prescribe weight-loss medications, especially if they’ve received training in obesity medicine. But not all are comfortable doing so. Many still lack the time, resources, or confidence to manage these treatments long-term. Specialized clinics or obesity medicine specialists are more likely to offer comprehensive care, including regular monitoring, nutrition support, and behavioral coaching. Ask your doctor if they’re certified in obesity medicine or can refer you to a program.
What if my insurance doesn’t cover it?
Insurance coverage for anti-obesity medications is still limited. If yours doesn’t cover it, ask the clinic about patient assistance programs offered by drug manufacturers. Some pharmaceutical companies provide free or discounted medication for low-income patients. You can also look into employer wellness programs-many now cover these treatments. In some cases, clinics offer sliding-scale fees based on income. Don’t give up-options exist, even if they require extra effort.
Are there side effects from these medications?
Yes, but they’re usually mild and temporary. Common side effects include nausea, constipation, or diarrhea-especially when starting or increasing the dose. These often improve within a few weeks. Serious side effects like pancreatitis or gallbladder disease are rare. Your provider will monitor you closely and adjust your dose if needed. The benefits of weight loss-reduced heart disease risk, improved diabetes control, better mobility-far outweigh the risks for most patients.

13 Comments
Medical weight management isn't about willpower-it's about biology. The fact that we're finally treating obesity like diabetes or hypertension is a huge step forward. I've seen patients go from needing oxygen just to walk to the bathroom to hiking with their grandkids. That's not magic. That's science.
So let me get this straight you're telling me the solution to obesity is just give people a 1000 dollar pill and call it a day? No wonder America's broke. People need to stop looking for shortcuts and just eat less and move more. This whole medicalization thing is just Big Pharma's latest hustle.
GLP-1 agonists? Sounds like a front for the government's bio-surveillance program. Did you know the original GLP-1 research was funded by the Gates Foundation and linked to WHO's Global Obesity Initiative? They're not curing obesity-they're creating dependency. The real data? Hidden. The side effects? Downplayed. Retatrutide? That's the third-gen version they're testing on low-income populations under the guise of 'clinical trials.' Wake up people.
OMG THIS IS SO TRUEEEEE!!! 😭 I tried dieting for 3 years and nothing worked... then I got semaglutide and lost 47lbs in 6 months!!! My jeans fit again!!! 🤩 My doctor said I'm 'reversing insulin resistance'-I didn't even know that was a thing!!! Thank you science!!! 🙏🙏🙏
They're calling it 'medical weight management' but it's really just another form of social control. Who decides what 'normal' weight is? Why are we pathologizing bodies that have existed for centuries? The real epidemic isn't obesity-it's the pharmaceutical industry's obsession with turning human variation into profit. And don't get me started on how they target women with 'lifestyle' ads while ignoring systemic food deserts and wage slavery.
The data presented here is methodologically sound and aligns with current clinical guidelines from the ACC and ADA. The distinction between medical and commercial interventions is critical. The 70% sustained weight loss metric in clinical settings versus 20% in commercial programs is not anecdotal-it's replicated across multiple longitudinal studies. Access barriers remain a public health crisis, but the framework for equitable delivery exists.
Look I've been in this game since the days of phentermine and cabbage soup diets and let me tell you something-nobody gives a shit about your BMI unless you're on Medicaid or your employer's insurance is trying to cut costs. The real issue is that doctors are too lazy to learn how to prescribe these new meds properly so they send you to some clinic that makes you watch a 45-minute video and then charges you $200 a month. Meanwhile my cousin in Texas just got a prescription from his Walmart doctor for $15 a month with no hoop jumping. The system is broken but not because the science is bad-it's because the bureaucracy is insane.
As a Latina woman who grew up eating arroz con pollo every Sunday, I can't tell you how relieved I am that my dietitian didn't tell me to stop eating my abuela's food. She helped me adjust portions, swap out fried for baked, and still let me enjoy family meals. That cultural respect? That's what made the difference. These meds helped me lose weight but the support helped me keep it.
The notion that obesity is a moral failing has caused generations of harm. It has led to delayed diagnoses, discriminatory treatment, and profound psychological trauma. The shift toward evidence-based, compassionate, multidisciplinary care is not just clinically effective-it's ethically imperative. We must expand access, eliminate bias, and center patient dignity. Anything less is negligence.
USA spending billions on fat pills while our veterans can't get mental health care? This is why we lost the economy. The elites want us fat and medicated so we don't protest. Just look at the stats-most of these clinics are in rich zip codes. Meanwhile my cousin in Ohio can't even get a referral. This ain't medicine. It's class warfare dressed in lab coats.
GLP-1 agonists = insulin mimetics = metabolic hijacking. The pharmacokinetics are well documented. The long-term safety profile is unknown. The weight loss is statistically significant but not clinically transformative for most. The real solution is caloric restriction with intermittent fasting. No pills needed.
Why are we even talking about this? The real problem is that Americans are weak. In my country we don't have these problems. We eat rice, we walk everywhere, we don't have soda machines in every school. This is a Western disease caused by capitalism and laziness. Stop spending money on pills and start teaching discipline.
They call it science but it's just another way to make people feel guilty for existing. You don't need a clinic to tell you your body is wrong. You just need someone to stop telling you you're broken. I lost weight without meds, without clinics, without shame. I just stopped listening to people who think my worth is tied to my BMI. Maybe the real treatment isn't in the prescription-it's in the silence.